
Coronavirus
Technology Solutions
June 4, 2021
Contractors Need
More Guidance on
Selecting Indoor
Air Treatment
Devices
Honeywell Shows
Value of Room
Purifiers for
Hotels
Indiana Approves
UV Light
Purification For
School Buses
School Buses are
Fifteen Times
More Crowded
Than a School
Room
Two Hundred
Kids
Hospitalized
with COVID in
First Quarter
Masks will be
Used for
Multiple
Purposes Post
COVID
___________________________________________________________________________
Contractors Need
More Guidance on
Selecting Indoor
Air Treatment
Devices
IAQ products
including MERV
13 filters, air
cleaners, UV
lights, and
bipolar
ionization have
been in high
demand. These
come with their
own sets of
challenges,
though, and they
may not always
be well suited
for each
application.
“Everyone's
defaulting to
MERV 13 or, in
some cases, HEPA
filters,
particularly in
the education
market,” said
Jeff
Littleton Exec.
VP of ASAHRAE
“A lot
of our design
engineers are
being asked by
their clients to
retrofit
existing systems
to put MERV 13
filters in, and
the pressure
drop behind the
filter can be an
issue. You have
to be really
careful, because
a key part of
fighting COVID
19 is to reduce
the
concentration of
pathogens in the
occupied spaces.
If you get less
ventilation
flowing through
that tighter
MERV 13 filter,
you can end up
with a bad
situation.”
While the demand
for IAQ devices
continues to be
high, there is a
lack of research
and standards
regarding the
efficacy of the
equipment.
ASHRAE is
planning to
rectify that
situation by
developing test
and design
standards for
various types of
IAQ products;
however,
determining the
appropriate
methods can be a
time-consuming
and complicated
proposition.
“Just think
about UVGI and
what kind of
tests are needed
for determining
dosage curves
for specific
pathogens across
a specific light
spectrum, for
example,” said
Littleton. “And
how does that
apply to various
mediums like
aerosols or
large droplets
or dry and wet
surfaces? And
how do you
commission a UV
antimicrobial
system in a new
or existing
facility? In an
air handling
unit or in
ductwork? So a
lot of
standards, and a
lot of research
is frankly
needed for all
of those
systems.”
To that end,
ASHRAE’s Board
of Directors
recently
approved the
title, purpose,
and scope (TPS)
for a new
standard,
entitled “Method
of Testing
In-Room Devices
and Systems for
Microorganism
Removal or
Inactivation in
a Chamber.”
While that is a
good first step,
Talbot Gee, CEO
of HARDI. is
concerned that
the standards
process will
take too long to
address some of
the problems
that are a major
concern right
now.
“Our
distributors are
bombarded daily
by new sales
pitches on new
products or
improved
products in the
IAQ space, and
their No. 1
frustration is
that they need
some way to
evaluate the
claims of all of
these products,”
he said. “It’s
easy to do for
energy usage on
a system, but
it's almost
impossible to do
for IAQ systems.
We don't have a
great way of
figuring out
which of these
IAQ technologies
is the real deal
versus snake
oil. My concern
is, we have a
generation of
contractors who
won't touch IAQ
with a 10-foot
pole, because
they're afraid
of getting
caught up in
something that
gets
misrepresented
or just doesn't
perform to its
stated claims.”
To combat that
issue, Gee would
like to see some
kind of
certification
program for IAQ
products or a
credible seal of
approval that
would be based
on performance
metrics.
“The standards
that ASHRAE is
working on are
going to be
fantastic, but
it's still
holistic, and it
doesn't
necessarily
specifically
help contractors
make a buying
decision on a
specific
product,” he
said. “We need
that next mile
to get done —
and frankly,
anything that
can be done to
accelerate it. I
fear that this
is kind of like
the pet rock fad
— there was a
short period of
time to sell the
pet rock before
it was gone. I'm
afraid if we
drag our feet
too long, that
some of these
IAQ technologies
might go that
route, and we
will have missed
our window and
not had a chance
to really grow
in that sector
of the economy.”
Littleton agreed
with Gee’s
assessment but
added that the
focus on IAQ
will continue to
be strong even
after the
pandemic.
“Memories tend
to be short, but
I do think in
terms of the
impact of the
pandemic, the
increased focus
on life safety
issues and
health issues —
as it relates to
IAQ — has legs.
It's going to
have a long-term
impact — a
permanent impact
on the way we
design systems
for buildings,”
he said. “ASHRAE’s
method of test
standard will
define how to
test the
efficacy of some
of this [IAQ]
equipment. Then
you do the
research, and
after that is
done, we’ll
develop design
standards that
define what is
the best way to
deploy some of
this equipment
based on its
efficacy and its
strengths and
weaknesses, and
so on.”
Due to the
increased
interest in this
particular
standard,
Littleton noted
that ASHRAE is
considering
allocating
additional
resources to
accelerate its
development, so
that it could be
available sooner
rather than
later. Still, he
noted that even
if its timeline
is moved up, the
standard will
not be finished
in time to help
people designing
buildings next
year.
“I don't think
it's a surprise
to anyone that
ASHRAE is not
the fastest
standards
developer on the
planet, but
we’re very, very
thorough,” he
said.
Honeywell Shows
Value of Room
Purifiers for
Hotels
The hotel
industry was
among the
hardest hit by
the pandemic. As
travel rates
increase, hotels
are turning to
science and
technology to
create
environments
that make guests
feel safer.
Honeywell
released
findings of a
computer
modeling study
that examined
indoor air
quality in hotel
common areas,
focusing
specifically on
filtration and
purification
methods used to
help mitigate
potential
airborne
contaminants.
The study found
that mobile HEPA
air purifiers
can help reduce
airborne
contaminants by
capturing
particles as
small as 0.3
microns and even
smaller. In
addition,
placing
purifiers in
high-traffic
areas is an
important factor
in reducing
contaminants.
The model
simulated
airborne
transmission
inside a common
area of a
select-service
hotel,
conditioned by a
traditional HVAC
system, to see
how far aerosols
travel and how
long they remain
suspended in the
air. Using
computer models,
the study
measured
airborne
particulates of
simulated
talking,
sneezing and
coughing in a
common area of a
hotel property,
such as the
dining area, and
the HVAC
system's
filtration
efficiency to
capture
contaminants
throughout the
space.
The
simulation
observed the
flow of large
and small
particles, taking
into account
factors such as
the location of
the HVAC supply
and return air
vents, air flow
physics, and the
social
distancing of
guests. In the
model, some of
the guests were
wearing face
coverings and
some were not
(i.e., to
simulate eating
in the dining
area). The study
specifically
examined the
impact of adding
mobile air
purifiers to
help pull
contaminated air
away from
guests.
Key Study
Findings: Air
Flow and Impact
of Air Purifiers
·
In the study,
97% of small
particles were
captured by air
purifiers, which
made a
significant
impact on the
improvement of
air quality.
·
Talking created
smaller and
fewer droplets
than a sneeze;
yet, when the
droplet attaches
itself to a
particle as an
aerosol,
dissemination
continued as
long as a person
talked and
traveled
approximately 60
feet in the
simulation due
to HVAC air
flow.
·
The closer a
source of
contaminants is
to the air
purifier, the
higher the
purifier's
effectiveness;
mobile HEPA air
purifiers
captured
particles as
small as 0.3
microns (and
smaller).
Key Study
Findings:
Effective
Placement of Air
Purifiers
·
Return air vents
are often at the
edges of a space
and, as a
result, can
allow aerosols
and other
particles to
travel farther.
Typically, HVAC
systems in
hotels and other
commercial
buildings are
not placed to
control
contaminants;
they are
designed for
comfort and
energy
efficiency by
controlling
temperature and
humidity.
·
Mobile HEPA air
purifiers placed
in strategic
locations in a
hotel lobby can
be effective in
managing the
spread of
contaminants,
large and small.
·
Air purifiers
that are less
obstructed and
set at tabletop
level were more
effective.
"People are
paying attention
to indoor air
quality,
especially as
they return to
public places,
and they want to
know that their
favorite
destinations are
taking
precautions,"
said Manish
Sharma, vice
president, chief
technology and
chief product
officer for
Honeywell
Building
Technologies.
"While this
computer
simulation
looked at how
hotels can
improve the air
quality in
places where
people
congregate –
like lobbies or
dining areas –
the learnings
can be applied
to other
environments
like schools,
dorms and office
conference
rooms. Modeling
suggests that
placing portable
air purifiers in
the exact places
that people are
can effectively
and quickly
filter the air
in a space
before particles
and aerosols
disseminate.
This study also
demonstrates
that improving
air quality
doesn't have to
be costly or
complicated -- a
good filtration
technology and
intentional
placement of it
can help remove
contaminants
from traveling
through the
air."
Background on
Air Purifiers
Standalone,
mobile HEPA air
purifiers are
known to capture
particles as
small as 0.3
microns and can
help reduce the
spread of
pathogens,
viruses and
contaminated
air. NASA
research
suggests
portable air
purifiers can be
effective at
removing
submicron and
nonparticulate
size matter as
well. Air
purifiers work
by pulling stale
air into the
unit where a
carbon filter
captures larger
particles, VOCs
and odors. The
air then passes
through the HEPA
filter, made of
tightly woven
glass or
synthetic fibers
to capture
smaller
particles
including smoke,
dust, pollen,
mold spores,
viruses and
bacteria.
Honeywell HEPA
air purifiers
offer building
owners a
cost-effective,
plug-and-play
solution that
does not require
infrastructural
changes.
Honeywell's Healthy
Buildings solutions
are part of a
comprehensive
effort to
innovate
solutions that
help critical
sectors of the
global economy
recover, like
hospitality,
without the need
to replace
existing
infrastructure.
Honeywell's
Healthy
Buildings
solutions
provide a
holistic view of
a building's
health based on
key factors such
as indoor air
quality,
occupant flow,
PPE analytics,
thermal
screening,
temperature
monitoring,
social
distancing and
sanitation
efficacy.
Honeywell
Building
Technologies (HBT)
says it is
transforming the
way every
building
operates to help
improve the
quality of life.
It is a leading
building
controls company
with operations
in more than 75
countries
supported by a
global channel
partner network.
Commercial
building owners
and operators
use its
hardware,
software and
analytics to
help create
safe, efficient
and productive
facilities. Its
solutions and
services are
used in more
than 10 million
buildings
worldwide.
Indiana Approves
UV Light
Purification For
School Buses
The Indiana
State School Bus
Committee
on June 1st,
2021, approved
the use of UV
light air
purification
systems
on Indiana school
buses after a
successful pilot
program
with Indiana based
Lumin-Air.
UV and MERV 13
Filtration on
School Bus
Andrew Desmarais,
Chief Operating
Officer of Lumin-Air
said, "This
approval is very
exciting
for Indiana school
districts and
puts Indiana on
par with other
states who have
already approved
these
technologies to
help provide
clean air in
their school
buses. Most
importantly Indiana schools
can now
implement a
solution to help
reduce the risk
of transmission
and better
protect
students, bus
drivers and
other school bus
occupants
against airborne
respiratory
pathogens like
SARS-CoV-2 and
Influenza."
School buses are
the most densely
populated areas
in a school's
facility and
typically have
the poorest air
quality. Lumin-Air's
system includes
MERV 13
filtration and
UV lights in an
enclosure,
circulating
clean,
disinfected air
throughout the
bus. This is a
much safer and
healthier
alternative to
opening school
bus windows,
which can bring
in unfiltered
air containing
exhaust,
allergens, and
particulates.
The U.S. Environmental
Protection
Agency (EPA)
urges limiting
inhalation of
diesel exhaust
especially for
children who
still have
developing
pulmonary
systems.
Timing for
approval was
critical
as Indiana schools
have until June
25th to turn in
proposals for
how they will
allocate the
large amount of
Elementary and
Secondary School
Emergency Relief
funds (ESSER) to
improve air
quality in their
facilities and
school bus
fleets.
Dan Fillenwarth,
President of
Lumin-Air
commented "If a
school system
spent a little
over 1% of their
ESSER funding on
air quality in
their school
buses they could
have systems
installed,
including
12-years of
replacement
filters and UV
bulbs,
addressing the
neediest portion
of their
facilities. This
would be a huge
step toward
improving the
health of
students,
teachers, and
bus drivers, and
helping to
protect schools
from shutting
down in the
future."
Lumin-Air has
successfully
installed their
solution
in California, Pennsylvania, Florida and Maryland,
on all major
school bus
manufacturer
models and on
two leading
metro bus
manufacturer's
vehicles. They
also have a
pilot program
underway on a
rail system.
School Buses are
Fifteen Times
More Crowded
Than a School
Room
The school bus
is an important
part of a
school’s
facilities,
where students
spend a
considerable
amount of their
daily school
time. School
buses are the
safest way to
travel to and
from school and
are the only
transportation
option for some
students.
School systems
are in the
process of
determining how
to best allocate
the large amount
of Elementary
and Secondary
School Emergency
Relief (ESSER)
funds, which
were made
available under
the American
Rescue Plan.
They’ve been
provided to
improve the
health of their
constituents,
and to ensure
that their
facilities are
prepared for and
avoid potential
closures. So,
let’s compare
the air in
school buses to
classrooms.
The Wells-Riley
model was
developed by
William F. Wells
and Richard L.
Riley in the
late 1970s to
quantify the
risks associated
with airborne
transmission of
respiratory
diseases. The
variables that
affect the rate
of infection
include time,
the infectivity
of the disease,
and the
concentration of
the infectious
particles. There
have also been
many recent
publications and
some excellent
computational
fluid dynamic
models showing
how the risk of
infection
increases as the
concentration of
contaminants
spreads within a
classroom.
Since we can’t
easily control
time or the
infectivity of
the disease, how
can we minimize
disease
transmission by
reducing the
“concentration”?
Concentration is
the number of
infectious
particles per
volume.
A typical
classroom for 25
students is
roughly 1,050
square feet with
a 9-foot
ceiling, or 378
cubic feet per
person. A
typical
77-passenger
school bus has
22 cubic feet
per person.
Imagine telling
your students,
teachers and
parents that due
to COVID-19, you
were going to
reduce the
capacity in one
of your
classrooms made
for 25 students
to 50-percent
capacity, and
that you’d still
fit 214 people.
You read that
right;
50-percent
capacity in your
school bus is
like 214 people
in a 25-person
classroom.
The American
Society of
Heating,
Refrigerating
and
Air-Conditioning
Engineers
(ASHRAE) and the
Centers for
Disease Control
and Prevention
(CDC) provides
some excellent
recommendations
on how to reduce
the
concentration of
contaminants
inside
classrooms. ASHRAE
62.1 Ventilation
for Acceptable
Indoor Air
Quality has
been adopted as
code throughout
the U.S. and
sets guidelines
for outside air.
A classroom
should bring in
10 cubic feet of
clean outside
air every minute
(cfm) for the
number of people
in that space,
plus 0.12 cfm
per square foot
of the space. In
our example,
that works out
to 500 cubic
feet per minute
of clean outside
air to dilute
indoor
contaminants in
the classroom.
ASHRAE 62.1 also
states that the
outside air
intake must be
more than 25
feet away from a
thoroughfare
with high
traffic volume,
like a bus
parking or
idling area.
If we applied
the same
criteria for the
classroom to the
school bus, we
would need 800
cubic feet per
minute of clean
air to dilute
contaminants in
the school bus.
How much clean
outside air do
we actually
bring into a
school bus? Even
if a bus has air
conditioning,
there is zero
outside air
induced through
it. Some buses
do have small
dash HVAC
systems that
bring in small
amounts of
outside air, but
the only outside
air that
typically comes
into a school
bus is through
an open window
or vent. Bus
drivers don’t
have control of
student’s
windows, so a
student can
close their
window because
of outside
conditions like
rain,
temperature and
noise—or for any
other reason
they want. The
quality of the
outside air
induced into the
bus is poor, as
bus windows are
hopefully never
more than
25-feet from the
road, or the
parking/idling
area as
prescribed by
ASHRAE.
Scientific
studies like “Reducing
Air Pollution
Exposure in
Passenger
Vehicles and
School Buses”
performed at the
University of
California, Los
Angeles point
out that high
levels of
traffic
emissions are
associated with
pulmonary and
cardiovascular
health risks,
especially for
children who
“are in the
developing stage
for pulmonary
function and
immune system.
In addition,
exposures to
particulate
pollutants were
also found to be
associated with
poor academic
performance.”
Amid a pandemic
and with no
better option,
it’s better to
open a window to
reduce
contaminant
concentration.
But the federal
government has
given us funds
so that we don’t
have to say, “We
don’t have
better options.”
If open windows
and vents are
not the best
options, what
else is
available? And
how does that
compare to the
classroom?
Again, ASHRAE
and the CDC
set guidelines
for classrooms.
The
recommendations
are simply to
improve filter
efficiency as
much as possible
and supplement
with ultraviolet
germicidal
irradiation,
especially when
outside air and
filtration
options are
limited.
ASHRAE
recommends a
minimum MERV-13
filter for the
reopening of
classrooms.
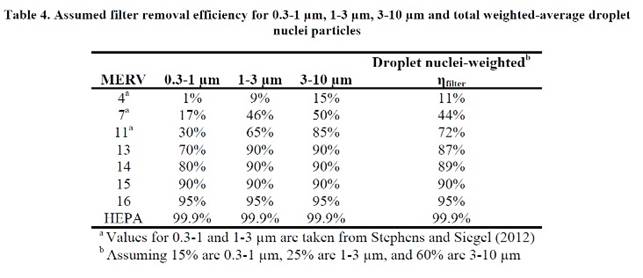
Filters are
rated on MERV
levels from low
to high, based
on the particles
that they
remove. Dr.
Brent Stephens
of the Illinois
Institute of
Technology
published a
report for the
National Air
Filtration
Association,
titled, “HVAC
filtration and
the Wells-Riley
approach to
assessing risks
of infectious
airborne
diseases.” The
report concludes
that MERV-13
filters remove
87 percent of
total droplet
nuclei expelled
during human
activities.
Typical bus
filters are
about MERV-2,
which are not
very effective
at removing
contaminated
particles. The
regular bus
filter is there
to try to keep
the coil clean,
not protect
humans.
To summarize,
the school bus
has the most
people per
volume of any
part of a
school’s
facilities. The
school bus also
has the lowest
amount and worst
quality of
outside air
available and
the poorest
filters.
The good news is
that there are
options
available for
school systems
to improve the
air in their
school buses.
Dr. William
Bahnfleth, chair
of the ASHRAE
Epidemic Task
Force, testified
in front of the
House Committee
on
Transportation
and
Infrastructure
earlier this
year. During his
testimony, he
said, “The
density of
people is
ordinarily much
higher than in
buildings. This
density
inherently
increases the
risk of
short-range
transmission,
and it is
difficult, if
not impossible,
to isolate
passengers.” He
also stated,
“Code minimum
ventilation and
MERV-13 filter
efficiency
should be viewed
as baseline
requirements
that may not be
sufficient. …
Air cleaners may
be used as a
supplement … The
best-established
technology (to
supplement
ventilation and
filtration)
currently is
disinfection
with germicidal
ultraviolet
light.”
If school
systems spent
1.2 percent of
their ESSER
money on
improving the
worst air in
their school
facility—the
school bus—they
could have a
system installed
including any UV
bulb and filter
changes for
12-years of
operation.
(Based on $190
billion in funds
for over 470,000
school buses.)
The device could
be removed from
buses no longer
in operation and
installed on new
buses.
Two Hundred Kids
Hospitalized
with COVID in
First Quarter
Over 200 kids
aged 12-17 were
likely
hospitalized for
COVID-19 from
January to the
end of March
across 14
states, with
over 31%
admitted to an
intensive care
unit and nearly
5% requiring
ventilator
support.
Coronavirus
hospitalization
rates in people
aged 12-17
increased during
March and April
in what the
director of the
Centers for
Disease Control
and Prevention
called a
"troubling"
trend.
The CDC
published a report on
Friday that
documented over
200 adolescents
who were likely
hospitalized for
COVID-19 across
14 states from
January to the
end of March. Of
those
12-17-year-olds,
over 31% were
admitted to an
intensive care
unit and nearly
5% required
ventilator
support. No
associated
deaths were
reported.
The agency also
found that the
hospitalization
rate in the age
group peaked at
2.1 per 100,000
in early
January,
declined to 0.6
in mid-March and
rose to 1.3 in
April. The
increased
hospitalization
rates could be
related to the
circulation of
highly
transmissible
variants, more
children
returning to
school and other
indoor
activities and
changes in
COVID-19
mitigation
measures,
according to the
report.
CDC Director
Rochelle
Walensky called
the data
"troubling"
during a press
conference on
Thursday.
"In the month
leading up to
the
recommendations
of the Pfizer
COVID-19
vaccines for
teens and
adolescents 12
and older, CDC
observed
troubling data
regarding the
hospitalizations
of adolescents
with COVID-19,"
she said. "More
concerning were
the number of
adolescents
admitted to the
hospital who
required
treatment in the
intensive care
unit with
mechanical
ventilation."
The Food and
Drug
Administration
in
May authorized
expanded use of
Pfizer's
coronavirus
vaccine in kids
aged 12-15.
Since then, the
Biden
administration
has urged
adolescents to
get vaccinated,
calling it the
"most important
thing you can do
right now."
Walensky said
the report's
findings "force
us to redouble
our motivation
to get our
adolescents and
young adults
vaccinated."
The majority of
the 204
adolescents
hospitalized
with the
coronavirus
across 14 states
from January to
March had one or
more underlying
medical
conditions,
including
obesity and
asthma. The
agency reported
that COVID-19
hospitalization
rates among
adolescents
exceeded
historical rates
of seasonal
influenza-associated
hospitalization
during
comparable
periods.
"Recent
increased
COVID-19–associated
hospitalization
rates in March
and April 2021
and the
potential for
severe disease
in adolescents
reinforce the
importance of
continued
COVID-19
prevention
measures,
including
vaccination and
correct and
consistent
wearing of masks
by persons not
yet fully
vaccinated or
when required by
laws, rules, or
regulations,"
the report said.
Masks will be
Used for
Multiple
Purposes Post
COVID
More than a year
into a pandemic
that has
sickened tens of
millions of
people in the
United States
and killed
more than
500,000,
most people are
eager to reclaim
some semblance
of their former
lives.
About half of
the country has
received at
least one
dose of
coronavirus
vaccines
authorized for
emergency use by
the Food and
Drug
Administration. Infection
rates are
dropping. And
federal health
authorities
have relaxed
mask
recommendations for
people
who are fully
vaccinated
against the
virus.
But it’s unclear
what our new
normal will look
like and
whether, at
least in some
form, it will
include face
coverings —
which have
been shown to
not only help
protect against
the coronavirus,
but also, with
additional
measures such
as social-distancing, slow
the spread of
influenza and
other
respiratory
diseases.
We’ve had
practically a
nonexistent flu
season this year
merely because
people were
doing the kinds
of public-health
things that were
directed
predominantly
against
covid-19,”
Anthony S. Fauci,
the nation’s
leading
infectious-diseases
expert, said
recently on
NBC’s “Meet the
Press.”
Even after the pandemic, Fauci said, it is “conceivable” that during certain seasonal periods when respiratory-borne viruses like influenza are more prevalent, “people might actually elect to wear masks” to keep from getting sick. Though polls show mask-wearing has declined as more Americans get vaccinated, a large number say they will continue sporting them, particularly in higher-risk situations, such as entering a crowded area.
It raises the
question: What
will the future
of mask-wearing
look like in
America?
Masks have been
used to prevent
respiratory
transmission of
infectious
illnesses in
health-care
settings for a
long time. In
fact, some say
the
strategy dates
to the Middle
Ages.
But it wasn’t
until the
early-20th
century that it
started to gain
more widespread
recognition as a
tool to prevent
disease.
A
Chinese-Malaysian
doctor named Wu
Lien-teh is
credited with
pioneering a
PPE-style mask
to protect
himself and his
team while
treating
patients during
the deadly
Manchurian
plague in the
early 1900s.
Fashioned from
gauze bandages
and wool, his
“anti-plague
mask”
helped protect
them from a
highly
contagious
disease that
killed scores of
people.
Mask-wearing
caught on in
many countries
in Asia as other
respiratory
epidemics
emerged. Even
today, some
Asians commonly
cover their
noses and mouths
to filter out
pollution or
protect others
from infection
when they are
ill, a practice
that became even
more pronounced
after the SARS
outbreak in the
early 2000s.
But absent major
respiratory
epidemics in the
West, the focus
shifted to
hand-washing to
try to guard
against
gastrointestinal
diseases, said
Jeremy Howard, a
research
scientist at the
University of
San Francisco in
California.
Everything
changed at the
start of the coronavirus pandemic
early last year.
Until then,
masking had been
an unfamiliar
concept in the
United States’
recent history,
at least when
used as a large
community-based
intervention.
Despite the politicization surrounding
masks, research
shows that
the strategy has
been a valuable
tool in the
fight against
covid-19,
helping to keep
people from
spreading germs
and protecting
others from
inhaling them.
Numerous studies
have shown that
masks reduce
infectious
respiratory
particles — the primary
method of
spreading the
coronavirus.
Masking,
especially when
practiced
alongside
hand-washing and
social-distancing,
has been
associated with
a decrease
in daily cases
and death
rates in
counties that
implemented mask
mandates,
according to
data from the
Centers for
Disease Control
and Prevention.
“It can really
be the
difference
between a mass
pandemic and
something that
kind of peters
out,” said
Howard, who
led a team of
international
researchers in
reviewing
evidence for
wearing masks.
That said,
Howard added
that the
increased
transmissibility
of variants
means that masks
and
social-distancing
may no longer be
enough, making
vaccines even
more crucial to
help slow the
spread.
Lisa Maragakis,
senior director
of infection
prevention at
Johns Hopkins
Health System,
said that over
the past year,
researchers have
amassed a wealth
of data on the
“incredible
power of
widespread
masking.”
“The question
is: What do we
do with that
information, and
also,
culturally, how
acceptable will
it be to people
to utilize this
tool even when
we’re finished
with the
pandemic?” she
said.
Maragakis
stressed that a
number of people
die of influenza
and other
respiratory
illnesses each
year in the
United States.
But, she said,
“one of the most
remarkable
things, in
addition to
interrupting
SARS-CoV-2
transmission, is
the fact that we
have seen almost
no influenza or respiratory
syncytial virus over
the past year.
That is yet
another aspect
we should really
think about,
because the
effectiveness
there has saved
tens of
thousands of
lives.”
The future of
masks
Although many
people are
itching to shed
their masks,
health experts
agree that even
after the
pandemic, people
who are sick —
with any
respiratory
illness — should
stay home when
possible. And
when they cannot
keep a distance
from others, it
may make sense
to mask up. As
to whether
people will do
that, some
experts doubt
it, but others
are hopeful
masking will
stick around, at
least in some
form.
Using masks on
public
transportation,
busy sidewalks
or in crowded
venues could
significantly
cut down on
illness,
particularly
during seasons
when respiratory
infections are
rampant. But
even if people
do not take
things that far,
they could
consider wearing
masks when sick,
Maragakis said.
“That would
certainly be a
time to wear a
mask — if you
have respiratory
symptoms and you
are continuing
to go somewhere.
That would be a
courteous and
preventative
measure to take
to prevent
transmission to
others,” she
said.
The majority of
more than 2,000
Americans
recently
surveyed said
they would
continue taking
precautions
after the
pandemic has
ended. In the
survey, from
Ohio State
University’s
Wexner Medical
Center,
90 percent of
respondents said
they would keep
up with frequent
hand-washing.
Eighty percent
said they would
still avoid
crowds. And 72
percent said
they intend to
keep wearing
their masks, at
least in certain
situations.
A recent Ipsos
poll showed
that 57 percent
were still
wearing masks
when leaving the
house, though
mask use “at all
times” has
declined about
10 percent among
those who are
vaccinated.
However, in an Economist/YouGov
poll released
last month, the
majority of
people who did
not plan to get
vaccinated were
more likely to
say that they
felt safe while
mask less. As The
Washington
Post’s Aaron
Blake reported,
the poll showed
that 63 percent
who intended to
forgo the
vaccine said
they felt at
least “somewhat”
safe socializing
indoors with
other
unvaccinated
people — without
wearing a mask.
Only 36 percent
of people who
had received at
least one dose
of the vaccine
said they felt
that way.
“I can tell you
that next
winter, when I’m
in crowded areas
like taking
public
transportation,
I, myself, will
probably wear a
mask so I can
prevent not just
covid but other
respiratory
illnesses as
well,” said
Bernard Camins,
medical director
of infection
prevention at
the Mount Sinai
Health System.
Some people will
be glad to see
the masks go.
But for others,
it may be more
complicated.
Clinical
psychologist
Lina Perl said
aside from
interfering with
how people
connect with
each other,
masks can also
become a “safety
behavior,”
resulting in
anxiety when the
mask is not on.
Since the
Centers for
Disease Control
and Prevention
started easing
masking
recommendations
for vaccinated
people, “we’re
in the process
of, ‘Okay, I’m
going to let
this go,’ and I
think people are
having a really
tough time,”
Perl said. “I
think people are
going to have to
push past that
anxiety and
practice not
using the masks
to get over that
safety
behavior.”
Yet, Perl said,
it’s a personal
decision and
people have to
find their own
balance.
“I think
everybody makes
different
choices about
how much risk
they’re willing
to take on,”
Perl said. “I
think that it
makes sense if
wearing a mask
is something
that fits into
your arsenal to
keep yourself
healthy.”
Experts said,
throughout the
pandemic, that
the reason for
wearing masks
has been not
only to protect
people out in
the community
but also to
prevent loved
ones at home
from contracting
the virus and
becoming
severely ill.
And the end of
the pandemic
will not
eliminate the
threat of the
coronavirus or
other
respiratory
infections.
“I think we
spend a great
deal of time and
effort and money
looking for
clinical cures
for diseases and
developing
vaccines and
other things,
but sometimes we
overlook the
simple things
that we can do
that can be
extremely
powerful. And I
think masking is
one of those
things,”
Maragakis said.
https://www.washingtonpost.com/lifestyle/2021/06/03/coronavirus-pandemic-future-masks/

