
Coronavirus
Technology Solutions
February 5, 2021
Breaking News in the Mask Webinar Today
Administration Considering Plan to Send Masks
Directly to American Households
Observed Face Mask Use at Six Universities —
United States, September–November 2020
Masks Are Needed After Vaccination
Safe Dining Program in Michigan
African COVID Cases Surge
Philadelphia Trying to Solve HVAC Challenge With
Fans
West Virginia County to Buy More Bipolar
Ionizers
CDC Position on Bipolar Ionization is That it is
Emerging Rather Than Proven
______________________________________________________________________________________
Breaking News in the Mask Webinar Today
There was a very useful exchange of information
in the webinar today. It includes some breaking
news.
Dave Rousse of INDA reported that ASTM has
surmounted the obstacles and will approve and
issue the mask standard in early March. The
structure remains as we have reported with two
efficiency levels.
Monica Ghandi of UCSF said “CDC told me
yesterday I am allowed to announce their MMWR
report is coming on Monday but didn’t share it
with me so I actually am not clear yet on what
it will say – but I think it is original
research on masks and advising which masks to
use with a variety of options to fit different
situations. Thanks to her tip, we are reporting
below on the University mask study released by
CDC today.
There were also comments during the discussions
that the Biden Administration is going to take
steps to insure that efficacious masks are
available.
All of these developments could indicate that
there are going to be ways to guide the
individual to choose the right mask. There is
going to be an effort by the government to see
that efficacious masks are used, and that is all
happening quickly.
Devabhaktuni Srikrishna of Patient Knowhow
provided details on a very valuable study
showing which masks are used and how they are
used in the U.S. His conclusion is that 85% of
the people are not using masks safely. By not
wearing masks safely outside their bubble they
bring back COVID to everyone in the bubble. This
study was covered in the Alert yesterday with a
link to the entire report.
There was a good exchange of information
relative to the availability of media and masks.
Dave Rousse told the group that the large
expenditures by media manufacturers assure
substantial production of meltblowns. He
pointed out that other non wovens are also
available and can meet a very large media
demand.
Lloyd Armbrust of Armbrust American
described testing they have done on KN95
masks.
The media was very inferior. However
imported surgical mask media was of higher
quality.
Lloyd is optimistic about the surgical
mask brace combination.
Per Lindblom of Hollingsworth & Vose is also
optimistic about the surgical mask-brace
combination.
His company has expanded its meltblown
capacity
The size of the market was discussed based on a
slide McIlvaine presented showing that the
public needs will be three times greater than
the medical needs even though the consumption
per capita is a fraction of the need by medical
workers.
The concept of masks and vaccines working in
tandem to create herd immunity was explored. In
the next six months in the U.S. masks can play
an even more important role than vaccines. Most
people will have been vaccinated in the U.S. by
autumn. So in the near term masks play the
dominant role but longer term they play a
subsidiary role to vaccinations.
For the 50% of the world with weaker economies,
vaccines will not be fully effective until
possibly 2024.
So masks can play the dominant role for
the next several years
The webinar can be viewed at:
https://youtu.be/tCij_ZiEOiE
Administration Considering Plan to Send Masks
Directly to American Households
The Biden White House is considering sending
masks directly to American households, according
to three people familiar with the discussions,
an action the Trump administration explored but
scrapped.
The Covid-19 Response
Team is evaluating the logistics of mailing out
millions of face coverings, but no decision has
been made, and the proposal hasn't yet reached
President Joe Biden for final approval, a White
House official said.
The idea has been raised in several meetings
among Biden's top health experts in recent days,
particularly as Biden continues to urge
Americans to use masks as a primary defense
against the spread of the
coronavirus.
Biden has asked all Americans to wear masks for
the first 100 days of his term, and he has
signed several executive actions that
mandate wearing face coverings on federal
property and aboard public transit, moves
President Donald Trump never enacted.
It's unclear when the masks would go out to the
public, how many would be included per residence
and whether they would be disposable or made of
cloth. It's also not yet clear what the cost
could be.
"There are a range of options on the table to
help protect more Americans from the coronavirus
and encourage people to mask up, but no decision
has been made," White House press secretary Jen
Psaki said.
A decision memo hasn't gone through the policy
process yet, a White House official said.
NBC News reported that the Trump White House scrapped
a plan last
year to deliver cloth masks to every U.S.
household, opting instead to send them to
nonprofit organizations and state agencies,
according to an internal email from a senior
administration official at the time.
The Department of Health and Human Services
signed $640 million in contracts in May with a
group of textile manufacturers to make masks
under Project America Strong, according to
federal purchase records. The largest contract
went to Hanes, which made 450 million masks in
May and July.
Dr. Anthony Fauci, director of the National
Institute of Allergy and Infectious Diseases,
said Wednesday that the Biden administration is
even weighing whether people should double-mask.
He indicated that it will wait for science to
guide its recommendations, but he said the key
is to wear at least one.
"If you're talking about a physical barrier and
as the CDC recommends, you want at least two
layers within the mask as a physical barrier,
and you feel maybe more of a physical barrier
would be better, there's nothing wrong with
people wearing two masks," Fauci said. "I often
myself wear two masks."
Observed Face Mask Use at Six Universities —
United States, September–November 2020
Early Release /
February 5, 2021
During September–November 2020, mask use was
directly observed at six universities with mask
mandates. Among persons observed indoors, 91.7%
wore masks correctly, varying by mask type, from
96.8% for N95-type masks and 92.2% for cloth
masks to 78.9% for bandanas, scarves, and
similar face coverings.
Approximately 41% of adults aged 18–24 years in
the United States are enrolled in a college or
university (1). Wearing a face mask can
reduce transmission of SARS-CoV-2, the virus
that causes coronavirus disease 2019 (COVID-19)
(2), and many colleges and universities
mandate mask use in public locations and
outdoors when within six feet of others. Studies
based on self-report have described mask use
ranging from 69.1% to 86.1% among adults aged
18–29 years (3); however, more objective
measures are needed. Direct observation by
trained observers is the accepted standard for
monitoring behaviors such as hand hygiene (4).
In this investigation, direct observation was
used to estimate the proportion of persons
wearing masks and the proportion of persons
wearing masks correctly (i.e., covering the nose
and mouth and secured under the chin*) on campus
and at nearby off-campus locations at six rural
and suburban universities with mask mandates in
the southern and western United States.
The participating universities included five
public universities with student populations
ranging from 29,000 to 52,000 and one private
university with a student population of 2,300;
five universities were in the South U.S. Census
region (two in East South Central and three in
South Atlantic), and one was in the West.
Approximately 10 student observers per
university were trained by one CDC staff member
who conducted training for all participating
universities using a standard protocol.† Universities
selected approximately 10 observation locations
where mask use was mandated.§ Indoor
mask use was mandated by all selected
universities and their surrounding communities.
Outdoor mask use was mandated when other
physical distancing measures were difficult to
maintain.¶ Observation locations
could be either indoors or outdoors; however,
because determining whether persons observed
outdoors should have been wearing a mask was not
always possible, the analyses focused on indoor
mask use. For up to 8 weeks (range: 2 to 8 weeks
across universities), observers tracked mask use
on varying days and times from fixed sites on
campus (e.g., libraries, classroom buildings,
dining facility entrances, student centers, and
lobbies of recreation centers and workout
facilities) and, at five universities, at nearby
off-campus, public locations frequented by
students (e.g., grocery stores, pharmacies, and
cafes). Observers modeled correct mask wearing,
remained inconspicuous, and refrained from
interacting with the persons they were
observing. Each observer was instructed to
record 40 observations at a single location or
to observe for 1 hour, whichever came first, for
a total of approximately 400 observations per
week per university by the 10 observers. Correct
mask use was recorded if the mask completely
covered the nose and mouth and was secured under
the chin. Observers were advised to record only
what they could see; for example, if a person’s
face could not be observed but mask straps were
visible behind the person’s head or ears, mask
use was recorded as “unknown.” Observers were
asked to remain stationary and record 1) whether
a mask was worn, 2) whether the mask was worn
correctly, and 3) the type of mask worn (cloth,
surgical, gaiter, masks that appeared to be N95
respirators [referred to as N95 type], or other)
for every third person passing a prespecified
location, such as a building entrance. If foot
traffic was too high to observe every third
person, observers were asked to select every
tenth person for the entire observation period (5).
Observation times varied during the mornings and
afternoons and at night and occurred on weekdays
and weekends. Because social groups might
exhibit more similar mask use behaviors, only
one person from a social group (e.g., an easily
identifiable family unit, group of friends, or
sports team) was sampled to avoid the effects of
clustering. Observers were instructed to observe
the first person in the group who corresponded
to the third person following the preceding
observation and then skip remaining group
members and resume counting every third person
after the group passed. Observations were
restricted to persons who appeared to be aged
≥12 years and were not limited to students. One
participating university released weekly media
reports highlighting their data from this
assessment to encourage mask use in their
community. A second university released a single
media report after 3 weeks of data collection.
The remaining four universities did not
publicize this investigation.
Mask mandates have been shown to decrease
SARS-CoV-2 case transmission,†† and
widespread mask use is a core intervention for
curbing the COVID-19 pandemic (6,7).
Direct observation at six universities indicated
that mask use was high on campuses in locations
where masks were mandated. Mask use was
similarly high at nearby, indoor off-campus
locations where masks were mandated. Mask use
was lower outdoors in areas where use was
mandated only when physical distancing could not
be maintained. These data provide evidence that
adherence to university mask mandates is high (5).
However, correct mask use varied by mask type.
Universities have several opportunities to
enforce policies such as mask mandates. For
example, universities could impose sanctions for
noncompliance with university policy.
Universities also could use multimodal education
and messaging to reinforce mask use, as well as
messaging specific to mask type and that is
focused on correct use. One university found
that having students sign a compact agreeing to
mask use, physical distancing, and testing might
also be effective in promoting these behaviors (8).
Observational investigations can provide rapid
feedback to universities on the prevalence and
type of mask use in their population. Using
trained student volunteers, participating
universities can quickly organize and collect
substantial amounts of data weekly at low to no
cost and review the data quickly to assess and
report on mask use. Universities and their
communities can use these data to tailor and
evaluate the effectiveness of messages and
education to reinforce and increase mask use and
to identify locations with lower adherence for
policy enforcement.
The findings in this report are subject to at
least three limitations. First, because the
period of observation ranged from 2 to 8 weeks
among universities, overall percentages are
influenced by the universities with more data.
However, all six universities are continuing to
collect data during the 2021 spring semester.
Second, observations were sampled without
recording information about the persons observed
and were not limited to university students,
staff members, or faculty members. Off-campus
locations likely included more persons not
affiliated with the university, and off-campus
percentages should be considered a measure of
community mask use. Finally, none of the
universities mandated outdoor mask use, unless
physical distancing could not be maintained.
Observers did not record whether physical
distancing was or was not maintained.
Compliance with CDC’s recommended COVID-19
mitigation strategy of mask wearing exceeded 80%
at six U.S. universities. Mask use is likely to
remain a critical COVID-19 mitigation strategy,
and CDC has made the training materials used in
this study available for universities that would
like to monitor mask use on their campuses.
However, in addition to mask mandates,
universities have implemented multicomponent
strategies that included reduced residential
density; surveillance and entry testing;
educational campaigns; and other campus and
community mitigation strategies. Monitoring mask
use, tailoring messages to promote healthy
behaviors (e.g., mask use, handwashing, and
physical distancing) on and off campus, and
developing measures to enforce or ensure
compliance with healthy behaviors have the
potential to improve implementation and
effectiveness of public health strategies to
protect persons on campus and in the surrounding
communities by preventing the spread of
SARS-CoV-2.
www.cdc.gov/mmwr/volumes/70/wr/mm7006e1.htm?s_cid=mm7006e1_w
Corresponding author: Lisa C. Barrios, LBarrios@cdc.gov.
Masks Are Needed After Vaccination
David Cennimo, an infectious disease specialist
for the Rutgers New Jersey Medical School, said
the most “pessimistic” reason why residents who
have been inoculated should continue wearing a
mask while in public and unable to social
distance is because they could be in the
minority of people for whom the vaccines are not
effective.
The Pfizer-BioNTech vaccine has been found to
prevent 95% of cases of the virus, and the
Moderna vaccine, 94.5% effective.
Beyond this reason, Cennimo said that it’s
significant to note that medical experts don’t
know that people who have been given the vaccine
can’t still transmit the coronavirus.
“I’m vaccinated, but I don’t know that I am not
infected with COVID,” Cennimo said. “I know that
I feel well; I know that I don’t have a fever.
But I could be harboring the coronavirus in my
nose right now; I could be breathing it out … so
because of that it’s still my responsibility to
wear a mask, because I don’t know that I’m
infection-free.”
“And that’s one of the hardest things to explain
to people, because if you got it in your head
that I just needed to get the vaccine and then
everything was going to be good, then we’re just
going to go back to normal, we don’t have the
data to tell you can go back to normal yet,”
Cennimo said.
It’s equally important to recognize that
immunity does not kick in immediately after
becoming vaccinated. It takes a week after the
second dose for the Pfizer-BioNTech vaccine to
become 95% effective. For Moderna’s vaccine,
efficacy reaches 94.5% two weeks after
become fully vaccinated, The
Washington Post reported.
“I even have friends in medicine who were like,
‘Oh, I want to go out to eat, I got my vaccine
today.’ I was like, “Please tell me you’re
joking,” Cennimo said. “You could go out to eat,
but you could have gone out to eat yesterday.
You got the vaccine in the last 24 hours;
there’s nothing different happening in your
body.”
At some point, but not in the immediate future.
While initially projecting that 60% to 70% of
the U.S. population must be inoculated to
achieve herd immunity, Dr. Anthony Fauci, the
director of the National Institute of Allergy
and Infectious Diseases and presidential
advisor, has since revised this language and
said that it may take closer to 90 percent
immunity to bring the coronavirus to a halt, The
New York Times reported.
Until then — even if you’ve been fortunate
enough to become vaccinated — wear a mask.
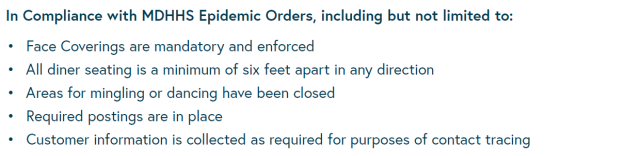
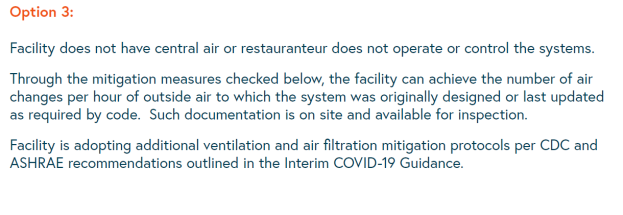
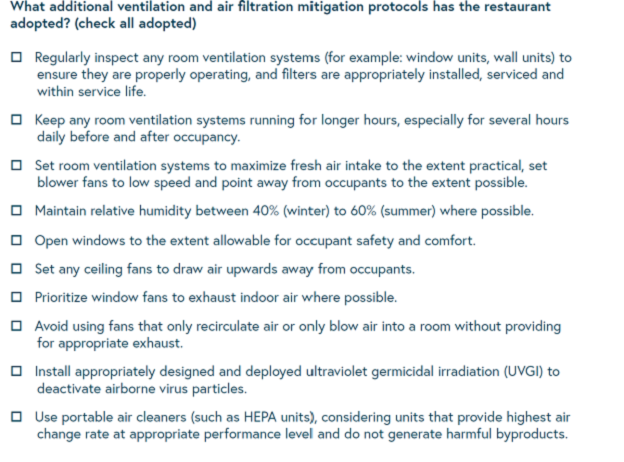
Safe Dining Program in Michigan
Many of the COVID-19 precautions restaurants can
take are quite visible, like sanitizing,
distancing and masking.
But a new state of Michigan program is pushing
restaurants to implement a safeguard that’s
harder for customers to see – improving
ventilation.
The MI
COVID-19 Safer Dining Program urges
restaurants to get an HVAC inspection and make
improvements to air filtration systems. COVID-19
is widely spread through airborne transmission,
meaning good ventilation and circulation can
help reduce the risk of spreading the virus.
The voluntary program launches just as indoor
dining is set to reopen, starting Monday, Feb.
1. It’s been closed since Nov. 18 because of a
second wave in the pandemic.
“We remain committed to helping businesses
implement processes and techniques to maximize
safety through layered mitigation strategies,”
said Michigan’s COVID-19 Workplace Safety
Director Sean Egan. “This program is another
opportunity for businesses to do just that.”
Restaurants that meet ventilation standards will
get a certificate to display publicly for
customers to see.
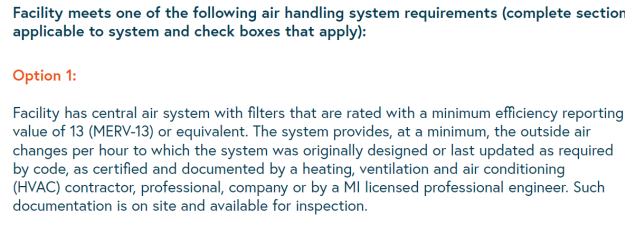
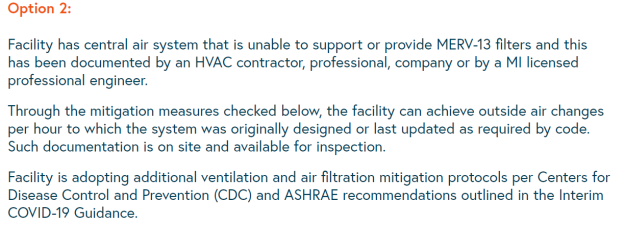
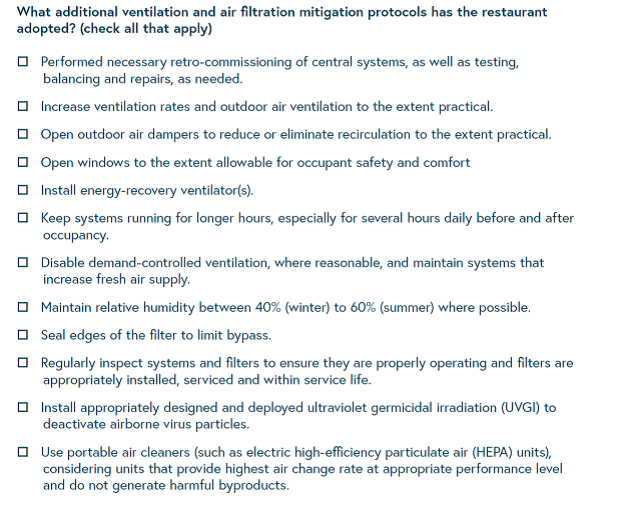
Some of the standards include having a MERV-13
filter or stronger and having a system that does
hourly air exchanges.
A contractor must sign off for a restaurant to
prove it meets the standards. Restaurants don’t
have to redo an inspection if one was done
recently, a state official said.
The businesses must cover the cost of the
inspection and any necessary upgrades if it
wants to get the voluntary certification. Gov.
Gretchen Whitmer’s proposed state funding
includes $10 million to pay for such inspections
and HVAC upgrades – however, the
package hasn’t been approved by the Legislature
yet.
The question is how much safer is a diner if a
contractor validates the restaurant compliance.
Here are items that need to be validated
African COVID Cases Surge
As African nations wait for hundreds of millions
of COVID-19 vaccine doses to arrive, health
officials are concerned about a general rise in
coronavirus cases and deaths, especially in
Southern Africa.
The stories, reported in local media and
highlighted by aid groups, are chilling. In the
tiny kingdom of eSwatini, medical aid group
Doctors Without Borders says health facilities
are seeing 200 new cases per day and a death
rate four times higher than they saw in the
first wave.
In the coastal nation of Mozambique, case
numbers are nearly seven times higher than they
were at the peak of the first wave in 2020.
And in the landlocked nation of Malawi, the
poorest country in Southern Africa, new cases
are doubling every four to five days, and the
nation’s main COVID-19 facility is nearly full.
Dr. John Nkengasong, head of the Africa Centers
for Disease Control and Prevention, tried to
break down the continent’s trajectory as many
nations enter a second wave without enough
vaccine supplies.
He said one indicator worth noting is that for
about a third of the continent’s countries, the
death rate has risen above the global average.
“It used to be the reverse,” he told reporters
via teleconference on Thursday. “During the
first wave, the case fatality rate was about
2.2%, and now we are seeing 2.6%. In terms of
the number of countries experiencing the second
wave, 41 of them are currently experiencing the
second wave on the continent. That is 41 of the
55 member states. Five countries accounted for
about 70%.”
Those countries are South Africa, Morocco,
Tunisia, Egypt and Ethiopia.
Africa escaped the worst of the pandemic last
year. But health experts point out the continent
now has many factors complicating the situation.
Testing has lagged behind the rest of the world.
Vaccine rollout has been slower, with just a
handful of countries only recently launching
vaccination campaigns.
And the continent’s chronic problems with
infrastructure and capacity mean that health
systems, social safety nets, transportation
networks and economies are struggling to meet
the challenge posed by this pandemic.
This, said Dr. Matshidiso Moeti, the World
Health Organization's (WHO) regional director
for Africa, is exactly what African health
officials have been talking about when they
warned against letting vaccine acquisition play
out in the open market, a situation that gives
wealthier nations advantages like having more
power to negotiate for cheaper vaccines in
larger quantities.
Moeti told journalists Thursday she was still
optimistic.
“Clearly, global solidarity is still a work in
progress,” she said. “It was our ambition. It
was our hope. It has not delivered to the extent
that we had hoped, but it is still a work in
progress. We are still doing our advocacy for
donations from countries that have secured more
vaccine to cover the entire population.”
Moeti said once African nations secure vaccine
doses, they face another challenge: convincing
people to take them. She emphasized that the
vaccines approved by WHO are safe and effective,
and said the organization is being proactive
about dispelling the growing tide of false
information about vaccines.
“What encourages me is that we know in the
African region that in general, people have been
positive about having their children
vaccinated,” she said. “It is only lately that
some of the anti-vaccine sentiments, messaging,
initiatives and campaigns have started to land
here. We need to build on African people's
belief in vaccines for their children to help
them to understand that something extraordinary
was done to develop these vaccines. And of
course, to be very factual about the fact that
we are learning about the vaccines as we go
along, but we know enough about their
efficaciousness.”
Moeti advised people who can take a WHO-approved
vaccine to do it. She and other experts
reiterated their best advice on containing the
coronavirus — stay at home, if possible, wear a
mask, wash hands and keep a safe distance.
Philadelphia Trying to Solve HVAC Challenge with
Fans
The following report on the status of
ventilation in Philadelphia elementary schools
is not encouraging. They will rely on 3000
window fans. It is well known that dilution is
not a very robust solution. In fact blowing
virus from one child to another even in a
diluted quantity is dangerous.
More than 30 public schools in Philadelphia have
either no ventilation system or a faulty one
that needs fixing, and some of those schools
will be part of a
Feb. 22 planning reopening for 9,000 elementary
school students.
The district will utilize window fans as the
main component at those schools to ventilate the
air in classrooms, and Superintendent William
Hite Jr. on Thursday defended the reopening. He
cited federal guidelines that approve of the air
flow provided by those fans and promised daily
monitoring in every classroom.
The 9,000 students returning to schools later
this month will be in kindergarten and the first
and second grades. It's the beginning of what
Hite hopes will be a phased return of all
students this school year even as the coronavirus
pandemic continues.
"It’s a temporary solution while we are getting
systems fixed and up and running again," Hite
said. "It goes back to the good faith efforts to
introduce fresh air into these spaces,
particularly those without ventilation."
Experts have said the fans proved able to
ventilate a classroom at standards set by the
U.S. Centers for Disease Control that allow for
up to 18 students in the room, Hite said.
"To date we’ve spent about $4 million on this
effort to get classrooms ventilated" and the
district is confident everyone will be safe,"
Hite said.
He pointed to other school districts, without
mentioning any by name, that have already
reopened in-person learning by simply opening
windows in classrooms.
Some parents and the city teachers' union is not
as convinced.
"Right now with those fans? One is risking it
all to send them to school," Philadelphia parent
Elizabeth Torres Pacheco told
station Telemundo 62, who translated her remarks
for this article.
She said she is not ready to send her sons back
to in-person learning yet.
Hite and other district officials have said
reopening will help students who have struggled
with digital learning and may feel isolated.
It is unclear exactly how many students have
failed to attend daily virtual learning classes,
but Hite said on Thursday that attendance is
similar to the first few weeks of the school
year in September when that figure stood at
about 80%.
In letters to parents,
Hite said
the district hired ventilation experts who
tested the air flow levels in "nearly every room
in every school district building."
The district is setting occupancy limits in
classrooms based on those tests, which measure
the volume of air circulating in the room in
cubic feet per minute. The rooms will follow a
safety standard of 15 cubic feet of outdoor air,
per person, per minute. The district says the
fans were tested to pump 270 cubic feet of air
per minute into rooms, allowing for 18 people in
a room.
Some other schools have had HVAC systems
repaired and can circulate enough air without
needing window fans installed, according
to the district's webpage.
Teachers told Telemundo 62 of concerns about
whether the fans will make classrooms cold, what
will be done during inclement weather, and if
the fans can last under constant use.
The district says it purchased 3,000 fans,
including extras in case replacements need to be
made later in the school year. The district
requires classrooms to be at least 68 degrees
and temperature tests have showed the room can
hold that temperature with the fans blowing air
in.
Other city leaders, including Councilmember
Helen Gym,
are concerned about ventilation at schools. The
Philadelphia Federation of Teachers said late
last month that the district was not keeping up
with a memorandum of understanding the union
sent. The union wants educators to be vaccinated
before returning to buildings - but Health
Commissioner Dr. Thomas Farley
said Tuesday that educators haven't yet been
called to receive the vaccine as the city works
through Phase 1B.
"I was surprised to learn when I got into this
that window fans can really make a big
difference in the amount of ventilation that
takes place," Farley told reporters in the
city's news conference on the pandemic Tuesday.
"We do think that this virus is spread in large
part, not entirely but in large part, through
the air, so if we increase ventilation that
should lower the risk," Farley said. "...If we
have an inexpensive solution, let’s use it."
West Virginia County to Buy More Bipolar
Ionizers
Ohio County W.V.
has set forth plans to attach technology
to ventilation in all school buildings that is
99.4-percent effective in preventing the spread
of COVID 19 molecules in school facilities.
The bipolar ionization boxes already are in
place at facilities receiving HVAC upgrades
through the school districts bond projects.
These include Wheeling Park High School,
Triadelphia Middle School and Elm Grove, Middle
Creek, Steenrod and West Liberty elementary
schools.
This week, the Ohio County Board of Education
approved a $100,000 expenditure with CMTA Energy
Solutions to bring the technology to more
facilities — Bridge Street Middle School,
Bethlehem, Ritchie and Madison elementary
schools, the Board of Education office and the
school district’s operations center.
The work will be completed in the next two to
three weeks, according to David Crumm,
administrator of operations for Ohio County
Schools.
Wheeling Middle School, the Warwood School and
Woodsdale Elementary School will receive their
bipolar ionization boxes moving forward as bond
work progresses.
Crumm explained the process of bipolar
ionization.
“What it does is it uses hydrolysis,” Crumm
explained. “Ions are sent out and attach to the
virus. That makes it so the receptors on the
virus cannot attach to anything else.”
The process doesn’t kill the COVID virus, but it
does make it inactive, he said. Research has
found it is 99.4 percent effective after 30
minutes.
Each school facility will require a different
number of the boxes, and Crumm isn’t certain as
to the individual price per box. It is likely
the school district will be reimbursed for the
expense through funding from the most recent
stimulus, he said.
CDC Position on Bipolar Ionization is That it is
Emerging Rather Than Proven
ASHRAE does not currently have a Society
position on bipolar ionization. However, the
ASHRAE ETF did reach out to CDC for their
position on the technology. The following is the
response from CDC in its entirety:
Thank you for your question. Although this was
pointed out in the earlier CDC responses, it is
important for me to re-emphasize that CDC does
not provide recommendations for, or against, any
manufacturer or manufacturer’s product. While
bi-polar ionization has been around for decades,
the technology has matured and many of the
earlier potential safety concerns are reportedly
now resolved. If you are considering the
acquisition of bi-polar ionization equipment,
you will want to be sure that the equipment
meets UL 2998 standard certification
(Environmental Claim Validation Procedure (ECVP)
for Zero Ozone Emissions from Air Cleaners)
which is intended to validate that no harmful
levels of ozone are produced. Relative to many
other air cleaning or disinfection technologies,
needlepoint bi-polar ionization has a
less-documented track record in regards to
cleaning/disinfecting large and fast volumes of
moving air within heating, ventilation, and air
conditioning (HVAC) systems. This is not to
imply that the technology doesn’t work as
advertised, only that in the absence of an
established body of evidence reflecting proven
efficacy under as-used conditions, the
technology is still considered by many to be an
“emerging technology”. As with all emerging
technologies, consumers are encouraged to
exercise caution and to do their homework.
Consumers should research the technology,
attempting to match any specific claims against
the consumer’s intended use. Consumers should
request efficacy performance data that
quantitively demonstrates a clear protective
benefit under conditions consistent with those
for which the consumer is intending to apply the
technology. Preferably, the documented
performance data under as-used conditions should
be available from multiple sources, some of
which should be independent, third party
sources.
