
Coronavirus
Technology Solutions
December 11, 2020
Vaccine
Purgatory and
Masks will be
the Reality for
the Next Year
Home
Disinfection
After Patient
Recovers
Key West Airport
will have a
Patrolling UV
Robot
LG Electronics
Robots Spray
Disinfectant or
Provide UV Light
More Efficient
Filters are More
Cost Effective
Than Outdoor Air
Dilution
Tennessee
Aquarium
Installs Ten New
HVAC Systems
____________________________________________________________________________
Vaccine
Purgatory and
Masks will be
the Reality for
the Next Year
Sarah Zhang of
the Atlantic
wrote that
we will be in
vaccine
purgatory for a
number of
months.
She
points out that
even with a 95%
efficient
vaccine it will
be wise to wear
a mask. Even a
5% risk makes
this effort
worthwhile.
The next six
months will
almost certainly
bring delays in
vaccine
timelines,
fights over
vaccine
priority, and
questions about
how immune the
newly vaccinated
are and how they
should behave.
We’ve spent 2020
adjusting to a
pandemic normal,
and now a
strange, new
period is upon
us. She calls it
vaccine
purgatory.
The biggest
unknown is how
long we will be
left in
purgatory.
Operation Warp
Speed officials
have laid
out an
aggressive
timeline to
get nearly all
Americans
vaccinated by
June, but this
presumes several
pieces going
perfectly. The
vaccines from
Pfizer, which
was just
recommended for
FDA
authorization,
and Moderna,
which is
expected to
follow next
week, cannot hit
manufacturing
delays, and
additional
vaccine
candidates, from
AstraZeneca and
Johnson &
Johnson, must
earn speedy
authorization
from the FDA
early next year.
Pfizer
earlier revised
down the number
of doses it will
deliver in 2020
and separately
has said it
cannot supply
any additional
doses to the
U.S., beyond the
100 million
already ordered,
before June. The
timeline for
authorizing
AstraZeneca’s
vaccine is up in
the air after
a messy clinical
trial. And
Johnson &
Johnson’s
has not yet been
proved to work.
Your experience
of this
purgatory may
depend on where
you live. While
a CDC
committee sets
recommendations
of how to
prioritize
initially scarce
doses, each
state ultimately
decides how to
allocate the
vaccines it
receives. A
person who
qualifies as an
essential worker
in Illinois
might not in
Indiana. One
city could end
up opening
vaccinations to
the general
public before
its neighbor.
This system is
meant to be
local and
flexible, but
that will
necessarily mean
a patchwork of
policies that
could come off
as unfair or
inconsistent.
“It is such a
complicated and
large logistical
challenge that a
lot of things
will go wrong. A
lot of things
will not go to
plan,” says Eric
Toner, a senior
scholar at the
Johns Hopkins
Center for
Health Security.
“The important
thing is not to
get hung up on
that.” Hard
trade-offs are
ahead, as many
groups have some
claim to
priority but
they by
definition
cannot all be
prioritized.
Toner says not
to lose sight of
the ultimate
goal: “Let’s
just keep
vaccinating
people.”
The decisions
still being made
about how to
prioritize
vaccines will
dramatically
color individual
people's
experiences over
the next months.
But ultimately
getting out of
purgatory will
require reaching
herd immunity,
which is
something we can
only achieve
collectively.
Vaccines can
protect
individuals, but
vaccination as a
public-health
strategy
protects a
community. Every
person who gets
vaccinated is a
small step
toward herd
immunity, toward
bringing down
the amount of
circulating
virus.
Eventually, we
can go all back
to schools and
dinner parties
and concerts.
Vaccines will do
very little to
change life for
the average
American in
2020. The very
first Americans
to receive
COVID-19
vaccines will be
health-care
workers and
residents of
long-term care
facilities.
These
priorities, set
by the CDC’s
Advisory
Committee on
Immunization
Practices last
week, are meant
to preserve the
health-care
system and to
save lives. People
in long-term
care facilities account
for many of the
hospitalizations
and roughly 40
percent of U.S.
COVID-19 deaths,
according to
data from the
COVID Tracking
Project at The
Atlantic,
even though only
a small fraction
of the country’s
population—less
than 1
percent—lives in
these
facilities.
Because the first shipments of vaccines will not cover all 24 million people in these two groups, the CDC has recommended sub-prioritizations too. Hospital workers who are in contact with patients are first on the list—including janitorial and support staff. The CDC also asks hospitals to consider that people who have recovered from COVID-19 likely have some immunity, so they do not need to be vaccinated first, though they won’t be prevented from getting vaccinated when doses are available later. For long-term care facilities, the CDC recommends putting skilled-nursing facilities, which have the sickest patients, before assisted-living facilities.
After
vaccination
begins,
hospitals and
nursing homes
will not change
overnight. Both
the Pfizer and
Moderna vaccines
require two
doses, three and
four weeks
apart,
respectively,
and even then
the vaccines
take time to
build
immunity—the
companies
measured 95
percent
protection from
COVID-19
symptoms only
after one or two
weeks. That will
be well into
2021 for even
the first people
vaccinated this
year. (The first
dose may offer some
protection after
10 days,
but that likely
wouldn't be as
strong or
long-lasting as
the full
regimen.)
Scientists also
do not yet have
the data to
confirm that the
vaccines
actually prevent
people from
spreading the
coronavirus
asymptomatically
in addition to
preventing
COVID-19
symptoms. This
is likely, but data
on this won’t be
available until
early next year.
For now, a
vaccine can
clearly offer
some protection
to the
recipient—but
that person
can’t be fully
confident about
not spreading
the disease to
others. A nurse
might feel safer
at work but
still worry
about bringing
the virus home
to their family.
Moreover, “even
with a vaccine
that is 95
percent
effective, you
don’t know if
you are in the 5
percent,” Marci
Drees, the
infection-prevention
officer at
ChristianaCare
and a
representative
on the CDC
advisory
committee,
points out.
Health-care
workers who come
in contact with
COVID-19
patients will
continue to need
full personal
protection
equipment. Drees
says she doesn’t
anticipate any
changes in PPE
or
quarantine-after-exposure
policies in the
near term.
Slowly, though,
small corners of
the world could
start to change.
In nursing homes
where every
staff member and
resident gets
vaccinated—essentially
reaching
building-wide
herd
immunity—some
restrictions
could be
loosened.
Residents could
increase their
very limited
socializing with
one another.
Jason Belden,
the director of
emergency
preparedness for
the California
Association of
Health
Facilities, says
the buildings
might eventually
open to some
visitors, but
symptom checks
and masking will
continue. With
everyone inside
vaccinated, the
risk from
unknowingly
letting in a
visitor who is
infected is
diminished, but
not zero.
The inclusion of
nursing-home
residents in the
first priority
group by the CDC
advisory
committee also
came as a bit of
a surprise to
states, which
did not expect
it when they
drew up vaccine
plans earlier
this year. The
federal
government
has contracted
with CVS and
Walgreens to
help vaccinate
nursing-home
residents, but
this division of
responsibility
between the
federal and
state levels has
also introduced
confusion.
Ehresmann says
she’s been told
to reserve some
number of her
state’s 183,000
initial
doses for
nursing homes,
even though the
nursing-home
vaccination
program also
won’t be ready
to start for a
few more weeks.
In California,
Belden says,
facilities in
the association
are still
waiting to find
out which ones
will get how
many doses when.
“All of our
members are
reaching out
every day. Am
I going to be
first? Am I
going to be
second? What's
it going to look
like? None
of those
questions have
been answered,”
he told me. “But
I do suspect
we’ll get
answers very
soon.”
Pfizer and
Moderna expect
to have 35 to 40
million doses of
their vaccines
ready by the end
of the year,
which is almost
enough to cover
hospitals and
nursing homes at
two doses per
person. By early
2021, states
will be getting
ready for the
next priority
group.
In some ways,
the very first
group is
actually the
easiest to
vaccinate.
Health-care
workers and
residents of
long-term-care
facilities are
relatively
well-defined
groups, and they
are already
concentrated in
hospitals and
nursing homes.
“The real test
will be what
comes after
that,” says Saad
Omer, a
vaccinologist
and the director
of the Yale
Institute for
Global Health.
It only gets
harder from
here.
The first hard
choice is a
stark one: Who
should come
next, essential
workers, or
adults over 65
or with
comorbidities?
The question
boils down to
which strategy
to prioritize,
Omer says:
reducing
transmission out
in the
community, by
vaccinating
essential
workers
interfacing with
the public, or
reducing deaths,
by vaccinating
the people most
at risk of dying
of COVID-19.
The CDC advisory committee has indicated that it will recommend essential workers next, though the National Academies and the World Health Organization have recommended the opposite. None of this guidance is binding. The decision is ultimately up to the states, though they have historically followed the CDC.
Essential
workers are also
a nebulous
category, and
again, states
get to set their
own definitions.
“There are an
awful lot of
interest groups
that are
lobbying states
and lobbying
feds to get
their members or
their
constituents
vaccinated
sooner,” Toner
told me. Should bank
tellers count
as essential
workers?
Teachers?
Exterminators?
And how should
states
prioritize
different groups
of essential
workers? One
study found
that 70
percent of
American workers can
be defined as
essential
workers and 42
percent as
frontline
workers that
directly
interact with
the public.
The decision to
prioritize
essential
workers also has
to do with
reaching
working-class
Black and Latino
communities that
have been
disproportionately
hit by the
coronavirus. But
these are the
same communities
that may be
hardest to
reach—because
of distrust
in the
government and
language
barriers. As
part of their
vaccine
planning, state
health
departments are
planning to
connect with
churches,
nonprofit
groups, and
other leaders in
those
communities.
Without this
effort, vaccines
will go only to
people who come
asking for it.
“The people who
are capable of
advocating for
themselves in
these situations
are sometimes
people who are
less in need of
the services
than those who
are not
advocating for
themselves,”
says Kelly
Moore, an
associate
director of the
Immunization
Action
Coalition. These
communities
might take
longer to reach,
which means the
overall
vaccination
might proceed a
bit slower.
There can be
tension, Toner
adds, between
vaccinating as
many people as
quickly as
possible and
actually
reaching
priority groups.
States and the
CDC are still
working out who
will qualify as
adults at high
risk for
COVID-19. Again,
there’s a
trade-off:
Requiring proof
will make
getting the
vaccines out
harder but
forgoing it
might mean
someone who
doesn’t strictly
qualify gets a
vaccine. “I
don’t think we
should get mired
in
documentation,”
Toner said. “I
don’t feel like
they should have
to show their
medical record
to prove that
they’re
diabetic. Or if
they say they’re
65, but they’re
only really 64,
I wouldn’t have
them bring a
birth
certificate. I
think to some
extent, we would
have to trust
people.”
When vaccines become available to the general public depends on a few unknowns. First, how many other vaccine candidates, like AstraZeneca’s and Johnson & Johnson’s, will actually also get authorized? These companies have already ramped up manufacturing, so doses can be ready to go as soon as the FDA gives the green light. Second, will they run into manufacturing delays? The mRNA vaccines from Pfizer and Moderna rely on a new technology that has never been used in an approved vaccine, let alone produced at the scale needed now. During manufacturing of the more routine H1N1 swine-flu vaccine during the 2009 pandemic, the U.S. ran out of “fill and finish” facilities that package bulk vaccines into vials. The government set up a program to prevent this bottleneck in the future, but other unforeseen snags may come up.
The last stage
of purgatory
will be getting
vaccines to the
general public.
Some parts of
the country may
allow everyone
to get the
vaccine sooner
than others. In
2009, says
Moore, who was
running
Tennessee’s
immunizations
program at the
time, demand for
the swine-flu
vaccine in
priority groups
varied across
the state. Some
vaccine
providers had
doses for
priority groups
sitting unused,
while members of
the general
public were
asking about
shots. Moore let
those providers
begin giving the
vaccine to
anyone who
asked. This
dynamic is very
likely to play
out between
cities and
between states
with the
COVID-19
vaccine, where
doses are
currently being
allocated by
census
population but
demand may vary.
This decision is
tough because
it’s likely to
be criticized
either way.
“Visualize the
frustration … if
Georgia and
Tennessee and
Alabama all have
different groups
being allowed to
be vaccinated at
different times.
But if you
don’t, if you
try to make
everyone in the
whole country do
these groups in
lockstep, then
you can imagine
that that also
is terribly
unfair,” Moore
says, if “there
are lots of
willing people
who could be
protected, and
vaccine is being
withheld.”
Vaccine
hesitancy is, of
course, also a
more general
concern across
the country. But
Americans’ willingness
to take a
COVID-19 vaccine
has risen as
data on the
vaccines’
efficacy have
come out, and
experts expect
it to keep
rising if early
vaccination goes
well. Many
people have said
they are more
comfortable waiting
a few months to
get the vaccine,
which is in
effect what will
happen.
Eventually, our
social lives can
start getting
back to normal.
It won’t happen
in a moment, but
stepwise, in
small ways and
then larger
ones. Omer says
small gatherings
like dinner
parties and game
nights might be
safe if everyone
in the group is
vaccinated.
School
reopenings and
mass gatherings
will likely
happen only when
widespread
vaccination—along
with masks and
social
distancing
through the
winter and
spring—pushes
COVID-19 rates
to low levels.
Public-health
experts stress
that vaccines
work in tandem
with other
measures: The
start of a
vaccination
campaign cannot
be an excuse to
abandon the
measures that
are working
right now. Moore
likens vaccines
to another slice
on a pile of
Swiss cheese,
where each slice
is an
intervention
that is by
itself imperfect
(masks, social
distancing, even
vaccines) but
they drastically
reduce risk when
stacked
together.
Rochelle
Walensky,
President-elect
Biden’s pick for
CDC director,
made
this analogy on
Twitter: “If I
have a cup of
water, I can put
out a stove
fire. But I
can’t put out a
forest fire,
even if that
water is 100%
potent. That’s
why everyone
must wear a
mask. As a
nation, we’ll
recover faster
if you give the
vaccine less
work to do when
it’s ready.”
There will
likely be many
frustrating and
imperfect things
about the
vaccine rollout
in the next few
months. But the
goal is to get
the country—and,
really, the
world—back to
normal, and that
happens not when
you as an
individual are
vaccinated but
when enough
people all over
are vaccinated.
It might take
longer than we
like, but we get
there together.
https://www.theatlantic.com/health/archive/2020/12/next-six-months-will-be-vaccine-purgatory/617371/
Sarah Zhang is
a staff writer
at The Atlantic.
Home
Disinfection
After Patient
Recovers
The COVID-19 pandemic
has spawned a
new business
that’s booming—
home
disinfection
services
It may be a job
for
electrostatic
disinfection. It
is used at
schools and
offices and is
now making the
rounds
after coronavirus hits
home.

(Photo: CBS2)
“It’s 360-degree
coverage. It
will get into
every crack and
crevice, much
better than a
surface wipe can
ever do,” said
Doug Baruchin of
I.T.S.
Environmental
Services.
Baruchin is a
certified
environmental
infection
control
remediator.
Homes get a full
wipe-down and
fogging with
peroxide- or
ammonia-based
products or
plant-based
disinfectants.
“It’s basically
the herb thyme
and it’s just as
effective on
coronavirus, but
safer for
aquatic life,
pets,” Baruchin
said. The
process takes
the work and
worry out of
returning a home
to health after
someone has been
sick.
But is this
overkill? CBS2’s
Dr. Max Gomez
says there is no
harm as long as
the disinfection
products are
safe. However,
he cautions,
“Surface
transmission
just isn’t a
high-probability
event. The CDC
has said its
really airborne
and that’s why
it’s so
important to
wear a mask.”
Sharntai Harris,
a Brooklyn
hairdresser who
recovered from
COVID-19, hired
Kristal Klean to
do what’s called
a “COVID
cleanse” of the
house she shares
with her mother
and child.
“This is
something that
kills COVID on
the surface, so
I want it
killed. I want
it out of my
house. I want it
away from my
loved ones,”
Harris said.
Disinfectant is
applied with a
sprayer for
customers who
simply don’t
want to go near
rooms that were
used for COVID
isolation.
“They treat it
like the red
zone, like ‘she
was up there,
you can start up
there.’ They
usually don’t
even go back in
until we come,”
Kristal Klean
owner Krystle
Vives said.
You can, of
course, follow
CDC guidelines
and carefully
disinfect your
own home, but
for services
starting at
$100, customers
say they’re
buying peace of
mind.
Electrostatic
disinfection
typically runs
around $300-$400
for a few rooms
but can go as
high as $1,500
for an entire
large house.
https://newyork.cbslocal.com/2020/12/03/coronavirus-covid-19-electrostatic-disinfection-homes/
Key West Airport
will have a
Patrolling UV
Robot
A coronavirus-fighting
robot is poised
to begin
patrolling Key
West
International
Airport’s
interior spaces
after hours
beginning
Tuesday,
December 15.
The robot emits
high-intensity
ultraviolet UV-C
wavelength light
that kills
harmful
pathogens in the
air and on
surfaces.
The ultraviolet
disinfection
robot, developed
by UVD
Robots,
is designed to
remove 99.9% of
pathogens
including
COVID-19. Key
West
International
Airport is among
the first
airports in the
United States to
acquire one of
the
sophisticated
units that
provides
non-chemical
disinfection,
according to a
manufacturer’s
representative.
The equipment’s
acquisition was
motivated by a
desire to
augment the
airport’s other
cleanliness and
passenger
protection
practices to
safeguard
against
coronavirus,
said Richard
Strickland,
director of
airports for the
Keys’ Monroe
County.
Airport
officials and
manufacturers’
representatives
demonstrated the
robot Wednesday
and Strickland
said Thursday
that the
manufacturer’s
representatives
should be
finished
programming and
training Key
West airport
staff by early
next week.
“Passengers
should know that
as they travel
to and utilize
the facilities
here, we’ve made
every effort
possible against
COVID-19 to
protect
passengers’
safety,” said
Strickland. “And
now, with the
ultraviolet
light robot that
we have here,
we’ll be able to
step that up
even another
notch.”
Standing nearly
6 feet tall and
weighing over
300 pounds, the
robot can move
around the
airport
autonomously
once it has been
programmed and
“mapped” spaces.
A human operator
is to ensure
people are away
from spaces the
robot will
sanitize and
monitors its
progress via an
electronic smart
tablet.
The robot’s
autonomous
operation is
vital, since the
light it emits
during the
active
disinfection
cycle is so
intense it can
only be used
after hours when
people are not
present. For
further safety,
a sensor will
shut the light
down if a human
presence is
detected to
protect people
from UV-C
exposure.
Officials said
the robot can
disinfect the
entire airport’s
interior spaces
in approximately
two-and-one-half
hours. Airport
officials are to
continue to
utilize other
efforts,
including manual
disinfection and
requiring that
all personnel
and passengers
wear masks, to
help mitigate
spread of the
COVID-19 virus.
Even with the
promise of mass
vaccination,
effective
disinfection is
still a key
element in
containing the
spread of
Covid-19.
Museums, theme
parks and other
attractions are
seeking ways to
ensure their
venues are as
safe as possible
and thorough
disinfection is
part of this
protocol. Robots
using UVC offer
large benefits
as effective
ways of
sterilizing not
just surfaces
but also the
air,
particularly in
indoor areas of
attractions.
LG Electronics
Robots Spray
Disinfectant or
Provide UV Light
LG Electronics
is set to
introduce the
CLOi robot at
the 2020 Korea
Electronics Show
being held at
the Digital
Innovation
Centre in Seoul.
The robot stands
160 centimeters
high and
contains panels
with
ultraviolet-C
(UVC) lamps. LG
claims it is
99.9 percent
effective in
killing bacteria
coliform and
staphylococcus
aureus from a
meter radius.
The robot has
autonomous
driving
technology
allowing it to
move easily
around
obstacles. LG is
also developing
a different
robot that will
spray
disinfectant
rather than use
the UVC lamps.
LG is not the
only company
with UVC
disinfection
robots. Xenex
has launched the
LightStrike robot
which can kill
99.9 percent of
SARS-CoV-2 virus
in two minutes
at a distance of
one meter.
“Pathogens have
evolved, but our
tools to clean
the environment
have not,” said
Mark Stibich,
chief science
officer and
co-founder of
Xenex. “We need
a new tool to
fight them, not
just a mop and
bucket.”
UVC is a form of
ultraviolet
light, shorter
than UVA and
UVB. It has a
wavelength of
between 100 to
280 nanometers
(nm). It is the
type of UV light
understood to be
most effective
at killing
germs, and is
commonly used to
disinfect,
surfaces, air
and liquids.
Different
wavelengths
disable viruses
in different
ways. The most
common
wavelength for
germicidal light
is 254nm which
damages the
viral DNA or RNA
so the virus
cannot
reproduce.
Meanwhile far
UVC (between 207
and 222 nm in
wavelength)
damages proteins
on the surface
of the virus so
it can’t attach
to human cells.
As Blooloop
reported
recently, many
companies have
been researching
and developing
applications for
UVC light and
these
innovations have
far-reaching
possibilities
for the
attractions
industry.
Recent studies
have shown that
UVC light can be
effective in
killing large
amounts of the
new coronavirus.
A study in The
American Journal
of Infectious
Control (AJIC) found
that UVC light
exposure
inactivated the
virus entirely
within nine
minutes. Another
study, also
reported in the AJIC found
that far-UVC
light reduced
live coronavirus
by 99.7 percent
in 30 seconds.
Disinfecting
robots are
efficient,
thorough and
time-saving.
However they
also offer
another major
benefit –
safety. UVC does
not appear to
cause skin
cancer or
cataracts (as
UVA and UVB can)
but doctors are
concerned that
it could affect
human eyesight.
Evidence shows
that far-UVC
light is the
safer form of
UVC light as it
doesn’t
penetrate beyond
the outer (dead)
layer of skin
cells and the
liquid film on
the eyes. Unlike
standard UVC, it
doesn’t cause
‘welder’s
flash’. Research
is underway on
the potential
effects on human
eyes. “I would
like to see more
research on
longer term
exposure before
I am convinced,”
said Karl
Linden,
professor of
environmental
engineering at
the University
of Colorado
talking the US
National
Institutes of
Health.
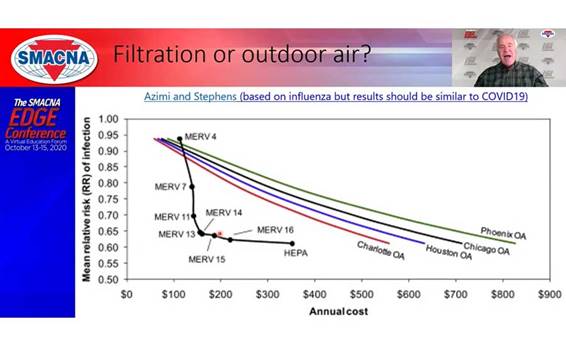
More Efficient
Filters are More
Cost Effective
Than Outdoor Air
Dilution
Since the start
of the COVID-19
pandemic, many
eyes have turned
to buildings’
HVAC systems to
help mitigate
the spread of
coronavirus
indoors. There
are a range of
options designed
to prevent the
virus from
traveling
through a
system. But how
effective are
they? At the
SMACNA Edge
event this fall,
Steve Taylor,
principal of
Taylor
Engineering in
Alameda,
California,
attempted to
answer that
question.
One of the
biggest
questions to be
answered: Which
is better at
preventing the
spread of
viruses —
filtration or
outside air?
Taylor said
there is plenty
of evidence that
more frequent
air changes
help, but that
air doesn’t have
to come from the
outside. A study
of the flu
offers some
insight into
which of the two
is more
effective. This
study finds that
filters are the
best defense.
And MERV 13
filters work as
well as higher
level filters.
Taylor said many
contractors
argue they
cannot place a
MERV 13 filter
into the 2-inch
space available.
They say the
pressure drop is
too tight as a
result. Taylor
said most
pressure drop
calculations are
conservative.
“If you had MERV
8 filters and
you replace them
with MERV 13
filters, it
would simply
work, fans would
speed up all by
themselves, and
you'd have
plenty of motor
horsepower to
handle it
because we
engineers are
very
conservative,”
he said. “So we
really think
that MERV 13 is
a very practical
requirement,
something that
most systems
will be able to
do without any
changes being
made.”
Filter Costs: During
his online
presentation for
the SMACNA Edge
event, Steve
Taylor shows the
effectiveness of
filters versus
increased
outside air in
preventing the
spread of the
flu. The risk
reduction with
outdoor air
introduction is
$700-$900
whereas a MERV
16 filter with
the same risk
reduction of
65 % is
only $250.
Another tool
promoted to
fight the virus
is UV lights.
Taylor said they
are effective,
but not
recommended for
air handlers. He
said better
filters are just
as easy to use,
less expensive,
and as effective
while using less
energy. The
filter housing
is already
there.
Some object that
filters only
capture the
virus rather
than kill it.
Taylor said
that’s untrue.
The virus dies
without a living
host.
What about
humidity? Taylor
said early
studies showed
that a higher
relative
humidity,
between 40% to
60%, helped
prevent spread.
Further studies
found little
effectiveness
from higher
relative
humidity.
“So all in all,
there's not
enough evidence
supporting
humidification
is a good
mitigation
measure,” Taylor
said.
Humidification
can also create
a lot of
problems on its
own, he said. It
can cause
condensation in
the ductwork
immediately
downstream of
the humidifiers,
as well as
humidification
within the
walls. If the
vapor barrier is
not in the right
place, it can
certainly cause
it on windows if
they're only
single glazed,
Taylor said.
“And wherever
there's
condensation,
there can be
microbial
growth,” he
said.
He concluded
that the best
solution for
improving an
HVAC system to
prevent the
spread of
coronavirus is
improving air
filters to MERV
13 or better.
Taylor said this
move has
benefits in many
parts of the
country, even if
the pandemic
ends. It
improves IAQ in
general and is
especially
useful when
regions are
dealing with the
smoke from
wildfires.
Of course, the
best filter is
the one closest
to a building’s
occupants — in
other words,
masks.
“There's no
practical amount
of ventilation
that's going to
protect you from
viruses unless
you have masks,”
Taylor said.
“They are
mandatory.
Tennessee
Aquarium
Installs Ten New
HVAC Systems
The Tennessee
Aquarium has
used a grant to
upgrade its HVAC
systems as a
safeguard
against the
indoor
transmission of
the virus that
causes COVID-19.
The aquarium in
Chattanooga says
it used an
$800,000
Tennessee
Community CARES
Program grant
from the state
Department of
Human Services
in part to buy
10 new HVAC
units. The
equipment has
ultraviolet
light filters
intended to help
disinfect the
air.
“The science
tells us that
increased
airflow and
better
filtration
greatly reduces
the risk of
exposure,”
Rodney Fuller,
the aquarium’s
director of
facilities and
maintenance,
said in a news
release. “As a
nonprofit, we
were grateful to
receive the
funding to add
another layer of
safety for our
guests, staff
and volunteers.”
The aquarium
reopened to
guests in June
under new health
protocols,
including mask
requirements for
guests older
than 12,
timed-entry
tickets and
capacity limits.
