
Coronavirus
Technology Solutions
November 25, 2020
CATE Basis for Mask Rating
Quantitative Fit Tests are Needed
Livestock Meat Packing Plants Responsible for
6-8% of COVID Cases in the U.S.
Meat Processors Not Using CATE Masks
CATE Masks Needed at Nursing Homes Now
______________________________________________________________________________
CATE Basis for Mask Rating
Masks should be selected based on a CATE rating
system which takes into account comfort,
attractiveness, tight fit and efficiency.
The rating can combine leakage
percentage, inefficiency percentage, and
resistance in mm H20 to produce a combined
rating number. Attractiveness could be A for
very attractive
B for medium and C for not attractive.
|
Mask |
Inefficiency % |
Leaks % |
Resistance mm H20 |
Total |
Attractiveness |
|
CATE mask 99 |
1 |
4 |
14 |
19 |
A |
|
CAE mask 95 |
5 |
4 |
9 |
18 |
A |
|
CATE mask 93 |
7 |
4 |
8 |
19 |
A |
|
Cloth Mask |
40 |
40 |
15 |
95 |
A |
|
Surgical Mask |
5 |
40 |
8 |
53 |
C |
|
LF N95 |
5 |
30 |
14 |
49 |
C |
|
TF N95 |
5 |
4 |
12 |
21 |
C |
This rating system will make it much easier for
people to select the best mask for their needs.
For example the numerical difference between a
18A mask and a
95A mask is striking.
On a rough basis the wearer can determine the
relative risk of one mask vs another. In a low
load virus environment the risk with the 18A
mask may be 1 in one thousand. The 95A
mask would generate 5.3 times that risk which is
still only 5.3 in one thousand. But in a super
spreader
situation where the odds jump
to 200 in 1000 or 20% with the 95A mask
they are only 3.8% for someone in a 18A mask
The inefficiency and leaks from various mask
types have been documented in previous alerts.
This includes loose fitting N95 masks
worn by a number of people who do not realize
the leak danger.
Testing firms such as Nelson Laboratories
already provide reliable validation of
efficiency and resistance
Fit testing for the public requires a different
system than for healthcare workers. For someone
in a hospital setting there are both qualitative
and quantitative fit testing methods. But they
require tests of individuals.
For masks used by the public the best approach
is to use a panel of people of different sizes,
provide appropriate masks for each and then test
leakage under various conditions.
One company has invested heavily in this
approach.
Vogmask has Quantitatively Fit Tested human
subjects to ensure the filtering efficiency is
retained over a series of motions like walking,
head movements, bending over, talking, etc. Here
is a sample of the fit testing on Test Subjects.
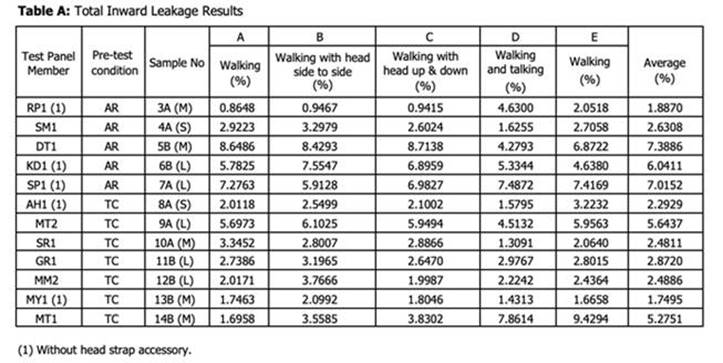
The determination of a leakage rating is
therefore more subjective and requires a
different validation approach. An expert
reviewing the Vogmask data would have confidence
that the leakage range is within the 1-8% range.
It is therefore recommended that a
validation group be formed to provide impartial
judgements on data submitted by mask makers.
This group can rely directly on leakage and
efficiency data if provided by a qualified firm.
It will need to spend more time reviewing the
fit data supplied by the mask maker. If this fit
testing is also done by approved vendors then
this too should require little time from the
validation group.
The validation group could charge for each mask
reviewed. The cost would not be appreciable if
the primary task is validation of the approach
used by others.
Quantitative Fit Tests are Needed
Examinetics explains the distinction between
qualitative and quantitative fit testing.
Qualitative fit testing is a pass/fail method
used on half-masks that relies on senses - such
as taste and smell - to detect air leakage from
your respirator. The half masks being tested
must have an overall fit factor (mask particle
concentration divided by the ambient particle
concentration) of 100 or less. The test relies
on a harmless, yet bitter-tasting chemicals
called Bitrex, which will determine whether you
pass. Rather than measuring the amount of
leakage into the facepiece, the qualitative fit
test determines whether the facepiece is in
working order. Unfortunately, if you taste a
bitter substance, it is a fail.
Specifically, at Examinetics, they offer taste
only tests. For those who cannot detect bitter
taste, they offer saccharin, an artificial
sweetener, as a replacement.
· Bitrex: a chemical that leaves a bitter taste
in your mouth
· Saccharin: a chemical that leaves a sweet
taste in your mouth
Workplace Quantitative fit testing is the
process to measure the precise amount of leakage
into any tight-fitting facepieces. Instead of
relying on bitter-tasting chemicals and your
senses, the test is performed by a machine
calculating the measurements. Typically, the
facepiece is attached to a probe, which is
connected to the measuring machine by a hose.
According to OSHA regulations, there are three
acceptable quantitative fit test methods:
· General aerosol
· Ambient aerosol
· Controlled negative pressure
Upon completion of the test, each eligible
employee has issued a card listing the make,
model and sizes of the respirator they received
a passed fit test.
Livestock Meat Packing Plants Responsible for
6-8% of COVID Cases in the U.S.
New research
published by
the National Academy of Sciences ties livestock
meat packing plants to 6% to 8% of U.S. COVID-19
cases, and 3% to 4% of the deaths through late
July.
The authors said the data show “a strong
positive relationship” between meatpacking
plants and “local community transmission,”
suggesting the plants act as “transmission
vectors” and “accelerate the spread of the
virus.”
Researchers at Columbia University’s School of
International and Public Affairs and the
University of Chicago’s Booth School of Business
found that the risk of excess death primarily
came from large meatpacking plants operated by
industry giants. Communities that acted to shut
down slaughterhouses reduced spread, according
to the researchers.
In a statement, the North American Meat
Institute said, "Meat and poultry companies
continue to invest, more than $1 billion so far,
in significant changes and improvements
regarding COVID-19 prevention and control
practices to protect the men and women who work
in their facilities. By limiting the data
examined to July 21, 2020, the article does not
evaluate the complete timeline of information.
The authors fail to capture the downward trend
of positive cases associated with the meat and
poultry industry into the summer and fall,
especially in contrast to the positive cases
reaching new highs around the nation.
"Significantly, even the authors suggest
caution, saying 'The best we can do here is
provide an unusually broad array of
observational evidence' and that they do not
want to 'overstate the hardness of our
method.' The timeline limitations, coupled with
those cautions, should give pause to drawing any
conclusions."
The peer-reviewed study was published last week
in the Proceedings of the National Academy of
Sciences of the U.S.
The researchers called the COVID-19 pandemic a
public health and economic crisis in which
policymakers face tradeoffs between maintaining
essential economic activities and mitigating
disease spread. President Trump issued an
executive order on April 28 directing
meatpackers to reopen closed facilities.
“Our study suggests that, among essential
industries, livestock processing poses a
particular public health risk extending far
beyond meatpacking companies and their
employees,” the authors wrote.
The study estimated packing plants were
associated with 236,000 to 310,000 COVID-19
cases and 4,300 to 5,200 deaths by July 21.
“The vast majority” of those cases were “likely
related to community spread outside these
plants,” the researchers wrote. The authors
suggested an investigation into supply chains,
operating procedures and labor relations within
the meatpacking industry.
The researchers also found plants that received
waivers from the U.S. Department of Agriculture
to increase their production-line speeds had
relatively more county-wide cases.
“Ensuring both public health and robust
essential supply chains may require an increase
in meatpacking oversight and potentially a shift
toward more decentralized, smaller-scale meat
production,” the study concluded.
Meat Processors Not Using CATE Masks
The following is the just revised guidelines for
meat processing plants in the state of Kansas.
they do not specify tight fitting
efficient masks and even allow workers to wear
cloth masks of their selection. They discourage
the use of medical masks.
Also since much of the transmission is
within worker families the use of CATE masks by
everyone would solve the problem
“Masks
for everyone entering facility: Employees should
wear a face mask/face covering at all times
while in the workplace. Employers can issue
facemasks or can
approve employees’ supplied cloth face coverings
in the event of shortages. At this time,
we are discouraging the
procurement of medical masks as they
remain in extremely short supply and should be
reserved for healthcare workers. All visitors to
the facility should also wear a face mask. Plans
and procedures should be in place to ensure 100%
mask use while in the facility. Health education
should be provided on the importance of masks”
CATE Masks Needed at Nursing Homes Now
Nursing homes workers who do not have COVID
patients can be using CATE masks. Nursing home
residents who do not have COVID should
definitely be using comfortable CATE masks.
Instead many residents are not wearing
masks and workers are reusing N95 masks for more
than one week. Here are some excerpts from an
NBC News Report.
More than 1,300 nursing homes across the U.S.
reported having three or more confirmed Covid-19
cases during the first week of November — the
highest number ever reported in a single week,
according to an NBC News analysis of federal
data. The figure does not include outbreaks at
assisted living facilities, which the federal
government does not track.
Many of the new nursing home infections are
emerging in the Midwestern states where the
virus is besieging the broader community,
including Illinois, Ohio, Missouri, Indiana,
Wisconsin and Iowa, which reported some of the
country's biggest weekly increases in suspected
and confirmed cases among residents, the data
showed. (Facilities report suspected cases when
residents exhibit Covid-19 symptoms but have yet
to receive positive test results.)
Nursing home case numbers have also been surging
in rural areas, with spikes in the Great Plains.
Facilities in South Dakota reported 253 new
infections among residents during the week that
ended Nov. 8 — three times the number reported a
month earlier. And across the country, a large
number of facilities are reporting staff
shortages, and some are still struggling to
acquire personal protective equipment and
reliable testing.
"It's an out-of-control fire. You stamp it out
in one place, then it pops up somewhere else,"
said Bill Sweeney, senior vice president of
government affairs at AARP, which
has urged Congress to pass more funding for
testing, personal protective equipment and
staffing for the country’s 15,000 nursing homes.
Friendship Haven, which runs a nursing home and
assisted living facility in Fort Dodge, Iowa,
had a few isolated Covid-19 cases over the
summer, but amid the state’s record surge, 12
staff members and 14 residents recently
tested positive.
"Masks are still not acceptable here,
and that is very frustrating. The community is
not really understanding," said Julie Thorson,
the president and CEO of Friendship Haven. "You
are worried about the inconvenience of a mask,
and my staff has been sweating and crying
through their masks since March."
New outbreaks are also emerging in facilities
that were pummeled by the first wave of the
pandemic — which killed tens of thousands of
residents in the Northeast and other early hot
spots — only for the virus to return.
Jewish Senior Services, a nursing home in
Bridgeport, Connecticut, had 22 residents die
from Covid-19 during the spring; about 10
percent of the staff became infected, said
Andrew Banoff, its president and CEO.
Personal protective
equipment was so scarce that the facility
resorted to purchasing supplies directly from a
company in China, he said.
Within a few months, cases finally subsided at
the facility and within the broader region. In
mid-June, Connecticut began requiring
weekly Covid-19 tests for all nursing home staff
members and residents and funded all the
testing. Other states have implemented similar
testing requirements, although not all are
paying for the tests.

Staff members with a resident of Jewish
Senior Services in Bridgeport, CN.
Jewish Senior Services
The nursing home was virus-free throughout the
summer and early fall. Then, in mid-October, as
case numbers began rising once again in
Connecticut, the first staff member tested
positive. Nineteen more staff members and eight
residents have become infected, as well, Banoff
said. Two of the residents died from Covid-19
last week.
"We knew we were on borrowed time," Banoff said.
"But it was devastating when we all had to go in
and call the families — not just of the
residents that tested positive, but those
exposed through staff. We had to make 84 phone
calls."
Jewish Senior Services and other long-term care
facilities have better access to testing and
personal protective equipment compared to the
spring. The federal government has
also distributed billions of dollars in Covid-19
relief funding to nursing homes, along with
rapid testing machines, although they are less
accurate than lab-based tests.
But nursing homes
across the country are still reporting shortages
of protective equipment and testing
delays. As of the first week of November 1 in 10
facilities said they did not have a week's
supply of N95 masks, according to the federal
data. Nearly a third of all nursing homes said
they had to wait three to seven days to receive
Covid-19 test results.
Providers worry that access to both protective
equipment and testing will become more difficult
as case numbers continue to rise.
The federal government unveiled new
testing guidelines in
late August, requiring staff members to be
tested monthly, weekly or twice a week,
depending on a county's overall positivity rate.
But nursing homes are still facing
difficulty getting access to tests, freeing up
staff members to administer them and covering
the cost, according to LeadingAge, an industry
group that represents nonprofit long-term care
facilities.
“Our pleas are being ignored. The support we
have received has been insufficient and is
running out quickly,” Katie Sloan Smith,
president and CEO of LeadingAge, said Monday on
a press call. “The virus is raging, infection
rates are skyrocketing, and the pool of
financial support is running low.”
The national stockpile — intended to be a
backstop for health care facilities that have
exhausted their supplies — is also facing
shortfalls. In July, the federal government said
it wanted to have a 90-day supply of critical
personal protective equipment on hand. As of
last week, however, the Strategic National
Stockpile had only about half of the 300 million
N95 masks needed and less than 1 percent of the
gloves needed to meet the target, according to
figures from the Department of Health and Human
Services.
Victoria Richardson, who earns $14 an hour as a
certified nursing assistant at a Chicago-area
nursing home
has been struggling to pay her bills since her
husband died of cancer in September, and she now
fears losing her home. She also still worries
about contracting the virus, which has killed 18
residents at Forest View since the beginning of
the pandemic. Even now, she said, staff members
struggle to get proper protective equipment. On
Monday, Richardson and nearly 700 other Infinity
nursing home workers went on strike to demand
higher pay and proper protective equipment.
"I have to reuse the
same mask for a week, and I don't get an N95
unless I insist on having it," Richardson said.
The Centers for Medicare and Medicaid Services
pointed to efforts to provide long-term care
facilities with testing, supplies, training and
technical assistance, but said that some nursing
home staff members were not following basic
Covid-19 protocols, like washing their hands and
wearing personal protective equipment properly.
“Based on our inspections and as the field
reports from our strike teams, we have found
that nursing home staff continue to fail to
consistently implement proper infection control
practices,” the agency said in a statement.
https://www.nbcnews.com/news/us-news/covid-19-outbreaks-nursing-homes-hit-record-high-n1248798
