
Coronavirus
Technology Solutions
November 10, 2020
CATE Masks Seven Times Better for Biden Mandate
PPE Demand Far Exceeds Supply but not if CATE
Masks Can Be Used
Biden Will Mandate Masks
Biden Lays Out COVID Program
_____________________________________________________________________________
CATE Masks Seven Times Better for Biden Mandate
The president elect in the U.S. is instituting a
mask mandate. This will be more effective if the
right masks are selected and worn.
CATE masks are seven times better than
cloth masks. They can be quickly made available.
The annual cost in the U.S. would be $30-60
billion/yr compared to $10-20 billion/yr for
cloth masks. The cost is insignificant compared
to the economic and social benefits. It is
important that the new Administration and people
around the world realize that the difference
between masks is as great as the differences
between pills.
CATE is an acronym for Comfortable, Attractive,
Tight Fitting, Efficient. These masks have been
available for many years to combat air
pollution, wildfires and pollen. they are the
ideal selection for the general public in the
fight against COVID.
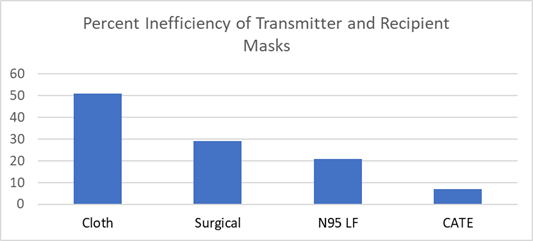
Here are the numbers.
In a room where people are social distancing at
six feet and MERV 8 filters are used in an HVAC
system with three air changes per hour unmasked
individuals will be generating a cloud of virus
particles similar to perfume or cigarette smoke.
If masks are worn by transmitters as well as
recipients, the net protection is a combination
of the performance of both masks.
|
Inefficiency of
Various
Combinations
Worn by Emitter
and Recipient |
||||
|
Parameter |
CATE |
Surgical |
N 95 unfitted |
Cloth |
|
Emitter |
|
|
|
|
|
Direct leakage |
4 |
30 |
20 |
30 |
|
Re-entrainment |
1 |
7 |
5 |
8 |
|
Penetration |
4 |
4 |
4 |
35 |
|
Inefficiency
Total |
9 |
41 |
29 |
74 |
|
% Captured
Ideal |
91 |
59 |
71 |
26 |
|
Use discount |
5 |
13 |
10 |
3 |
|
Net Capture % |
86 |
46 |
61 |
23 |
|
Recipient |
|
|
|
|
|
Recipient Load |
14 |
54 |
39 |
77 |
|
In leakage |
1 |
15 |
8 |
22 |
|
Penetration |
1 |
3 |
2 |
27 |
|
% captured |
12 |
36 |
29 |
28 |
|
Net efficiency |
98 |
82 |
89 |
51 |
|
Use discount |
5 |
11 |
10 |
2 |
|
Effectiveness |
93 |
71 |
79 |
49 |
|
Inefficiency |
7 |
29. |
21 |
51 |
The net effectiveness is a function of the
potential capability of the mask minus failure
to achieve a tight fit and periods where the
mask is discarded due to discomfort or social
drivers. When all is considered the CATE mask
combination is 93% effective compared to only
49% for the cloth mask.
Mask type: CATE masks are generally reusable and
have various features to make them
attractive, tight fitting and comfortable
as well as efficient. Surgical masks are
efficient but not tight fitting. N95 masks
can be fitted for a tight seal but when
worn by general public they are often not used
properly.
Cloth masks can excel in comfort and
attractiveness but are loose fitting and
inefficient.
Direct Leakage: This is the amount of air which
is exhaled around the mask directly.
Re-entrainment: Droplets initially captured on
masks evaporate and split causing virus to
escape.
Penetration:
This relates to the efficiency of the
filter media.
Use Discount:
Masks should be worn as appropriate.
Cloth and CAT masks are more comfortable than
the others and are more likely to be used in
borderline situations.
Recipient Load: This is the virus escaping the
transmitter mask.
In Leakage: This is the amount inhaled around
the mask seals.
There is no question that tight fitting
efficient masks are the most effective weapon
against COVID. These masks prevented any
U.S. medical staff fighting Ebola to
become infected. The COVID incidence among
medical personnel in high COVID environments is
very low. In cases where these personnel had no
choice but loose fitting surgical masks the
infection rate was high. If a comfortable,
attractive version is available to the general
public the battle can be easily won.
PPE Demand Far Exceeds Supply but not if CATE
Masks Can Be Used
This is the conclusion of many including CBS
Money Watch.
But this is assuming that disposable melt
blown surgical and N95 masks cannot be replaced
by reusable CATE type masks for healthcare
applications. In fact in any healthcare
environment where the
virus load is not likely to be greater
than the virus load in the community, the CATE
masks are a better choice.
This would include nursing homes,
hospital reception areas and most areas other
than emergency rooms and areas of the hospital
where infectious patients are being treated.
3M Company, the largest domestic manufacturer of
N95 masks told CBS MoneyWatch that "U.S. and
global demand for PPE continues to far exceed
supply for the entire industry."
Some of 3M's health care clients are using 20
times the amount of PPE they needed before the
pandemic, a company spokesperson said. 3M is
also fielding requests for respirators from new
clients that have never used them before. Some
suppliers report a jump in sales in states where
COVID-19 cases are rising.
3M's monthly production of N95 respirators in
the U.S. alone will have increased from 22
million in 2019 to 95 million by the end of
2020, a spokesperson said. Globally, by the end
of 2020, the company will have produced 2
billion respirators.
That's still not enough: Nine months into the
pandemic, manufacturers are still limiting how
many masks may be purchased, including for
hospitals.
In health care settings, as a rule of thumb,
facilities should stock at least a 90-day supply
of masks at all times, according to experts and
some state health departments. But many cannot.
MidMichigan Health, a nonprofit health system in
Michigan, only has about 30 days' worth of masks
on hand.
"We can't build to a 90-day supply at this point
because the demand is going up across the
country, which is basically what happened back
in February right after all this started," said
Jeff Wagner, the vice president of materials
management at MidMichigan Health.
A three-month supply would be ideal given that
case numbers are rising. "If we can get there,
we could ride out the storm for a little bit. A
90-day supply of good-quality product would make
me very happy," Wagner said.
But rising case numbers in central Michigan will
only make it harder to secure the goods. "It's
just going to get tougher and tougher," he
added.
MidMichigan, with hospitals, physician
practices, urgent care and other centers serving
938,000 Michiganders, is coping with the
shortfall by disinfecting the masks it has using
UV light to prolong their usefulness.
"There are safe ways to disinfect masks but it's
very time-consuming. It's not the ideal solution
by any means," said Awi Federgruen, a production
and supply chain management expert and professor
at Columbia University Business School in New
York.
Part of the reason for the bottleneck in
production stems from the complex process by
which NIOSH-certified N95 masks are made. Though
prices vary based on quantities purchased,
buyers can expect to pay between 50 cents and
one dollar per respirator, according to sellers.
"It's a pretty difficult item to manufacture,
particularly the main filter. It requires
specialized machinery that's very expensive,"
Federgruen said.
Brian Wolin, whose work as a chiropractor dried
up when he was forced to stay home at the
beginning of the pandemic, is trying to help
meet hospitals' mask needs. Since August, his
company, Protective Health Gear in Paterson, New
Jersey, has been making and selling CDC-approved
N95 masks.
The company can now make up to 1.4 million masks
per month, and it plans to increase production
by year-end.
"We've started to feel the phone calls and
emails escalating as the case numbers creep up,"
Wolin said. "We're not sold out yet, but we have
to ramp up production."
Health officials in Montana, New Mexico and
Wyoming also expect supplies to tighten in the
coming weeks as cases rise and demand for masks
increases, according to a Wall Street
Journal report.
In addition, thousands of nursing homes cite
shortages of PPE, including masks, according to
a recent report from the U.S. Public Interest
Group. a consumer advocacy group.
In August, seven months into the pandemic, 20%
of nursing homes had a less-than-one-week supply
of one or more types of PPE, according to the
report. which represents a critical shortage by
industry standards.
"It's critical because an outbreak could wipe
out their supply in a day or two," wrote U.S.
PIRG's Teresa Murray and Jamie Friedman of
Frontier Group, the report's co-authors.
Columbia's Federgruen says part of the problem
is matching PPE supplies with demand around the
U.S. "The level of organization is dismal in
terms of knowing where people are holding and
who can we make contracts with across the globe.
It's still very much in its infancy."
Mike Bowen, vice president of Prestige
Ameritech, which sells bulk quantities of N95
masks to hospital distributors, is among the
suppliers that actually have a surplus on hand
after more than tripling his employee headcount
to boost mask production.
"We are looking for more hospitals that are in
trouble. If there are hospitals that are in
desperate need of respirators, we have them. We
have excess capacity of N95s and of face
shields," he said.
Biden Will Mandate Masks
President-elect Joe Biden will personally call
on governors around the country to enact mask
mandates in their states once taking office next
year, NBC
News first
reported on Sunday.
A Biden campaign official told the network that
governors who resist the incoming president's
requests will see Biden pressure mayors of
cities in their respective states to enact
mandates at the local level, potentially setting
him up for confrontations with Republican
governors around the U.S.
“If a governor declines, he’ll go to the mayors
in the state and ask them to lead,” said the
official, according to NBC. “In many states
there is the capacity of mayors to institute
mandates.”
More than 20 states currently require masks to
be worn in private businesses and public places
according to an NPR tally, and Biden has called
for more governors to enact such mandates for
months as case numbers have exploded around the
U.S. with the fall.
Anthony Fauci, a top member of the White House
coronavirus task force, has also expressed
support for a national mask mandate.
Biden Lays Out COVID Program
The U.S. can expect increased Covid-19 testing,
a national mask policy and the possibility of
nationwide lockdowns once President-elect Joe
Biden takes office Jan. 20. Here is the plan he
introduced previously.
The American people deserve an urgent, robust,
and professional response to the growing public
health and economic crisis caused by the
coronavirus (COVID-19) outbreak. That is why Joe
Biden is outlining a plan to mount:
·
A decisive public health response that ensures
the wide availability of free testing; the
elimination of all cost barriers to preventive
care and treatment for COVID-19; the development
of a vaccine; and the full deployment and
operation of necessary supplies, personnel, and
facilities.
· A decisive economic response that starts with emergency paid leave for all those affected by the outbreak and gives all necessary help to workers, families, and small businesses that are hit hard by this crisis. Make no mistake: this will require an immediate set of ambitious and progressive economic measures, and further decisive action to address the larger macro-economic shock from this outbreak.
Biden believes we must spend whatever it takes, without delay, to meet public health needs and deal with the mounting economic consequences. The federal government must act swiftly and aggressively to help protect and support our families, small businesses, first responders and caregivers essential to help us face this challenge, those who are most vulnerable to health and economic impacts, and our broader communities – not to blame others or bail out corporations.
Public health emergencies require disciplined, trustworthy leadership grounded in science. In a moment of crisis, leadership requires listening to experts and communicating credible information to the American public. We must move boldly, smartly, and swiftly. Biden knows how to mount an effective crisis response and elevate the voices of scientists, public health experts, and first responders. He helped lead the Obama-Biden Administration’s effective response to the 2009 H1N1 pandemic and the 2014 Ebola epidemic. Biden also helped lead the response to the greatest economic crisis since the Great Depression and ran point on implementation of the Recovery Act. He knows how to get relief out the door to families, as well as resources to state and local officials to deal with the challenges they are facing.
And, even as we respond to this crisis, we must prepare for the next one. As President, Biden will establish and manage a permanent, professional, sufficiently resourced public health and first responder system that protects the American people by scaling up biomedical research, deploying rapid testing capacity, ensuring robust nationwide disease surveillance, sustaining a first class public health and first responder workforce, establishing a flexible emergency budgeting authority, and mobilizing the world to ensure greater sustained preparedness for future pandemics.
Congress has taken a step forward by passing an initial bipartisan emergency plan to combat COVID-19. The Trump Administration must now heed the calls of House Speaker Nancy Pelosi and Senate Democratic Leader Chuck Schumer to put the health and safety of the American people first. Much more needs to be done, now, to bring our country together, respond to this emergency, and set the groundwork for bold, long-term reforms, including ensuring quality, affordable health care and a comprehensive paid leave program for every American.
Biden will be ready on Day One of his
Administration to protect this country’s health
and well-being. But he is not waiting until then
to communicate his views on what must be done
now to properly serve the American people. Biden
believes the following steps must immediately be
taken.
The Biden Plan calls for:
·
Restoring trust, credibility, and common
purpose.
·
Mounting an effective national emergency
response that saves lives, protects frontline
workers, and minimizes the spread of COVID-19.
·
Eliminating cost barriers for prevention of and
care for COVID-19.
·
Pursuing decisive economic measures to help
hard-hit workers, families, and small businesses
and to stabilize the American economy.
·
Rallying the world to confront this crisis while
laying the foundation for the future.
Biden understands that this is a dynamic
situation. The steps proposed below are a start.
As the crisis unfolds, Biden will build on this
policy to address new challenges.
RESTORING TRUST, CREDIBILITY, AND COMMON
PURPOSE
Stop the political theater and willful
misinformation that has heightened confusion and
discrimination. Biden
believes we must immediately put scientists and
public health leaders front and center in
communication with the American people in order
to provide regular guidance and deliver timely
public health updates, including by immediately
establishing daily, expert-led press briefings. This
communication is essential to combating the
dangerous epidemic of
fear, chaos, and stigmatization that can
overtake communities faster than the virus. Acts
of racism and xenophobia against the Asian
American and Pacific Islander community must not
be tolerated.
Ensure that public health decisions are made by
public health professionals and not
politicians, and
officials engaged in the response do not fear
retribution or public disparagement for
performing their jobs.
Immediately restore the White House National
Security Council Directorate for Global Health
Security and Biodefense, which
was established by the Obama-Biden
Administration and eliminated by the Trump
Administration in 2018.
MOUNTING AN EFFECTIVE NATIONAL EMERGENCY
RESPONSE THAT SAVES LIVES, PROTECTS FRONTLINE
WORKERS, AND MINIMIZES THE SPREAD OF COVID-19
Make Testing Widely Available and Free
Ensure that every person who needs a test can get one – and that testing for those who need it is free. Individuals should also not have to pay anything out of their own pockets for the visit at which the test is ordered, regardless of their immigration status. The Centers for Disease Control and Prevention (CDC) must draw on advice from outside scientists to clarify the criteria for testing, including consideration of prioritizing first responders and health care workers so they can return to addressing the crisis.
Establish at least ten mobile testing sites and drive-through facilities per state to speed testing and protect health care workers. Starting in large cities and rapidly expanding beyond, the CDC must work with private labs and manufacturers to ensure adequate production capacity, quality control, training, and technical assistance. The number of tests must be in the millions, not the thousands.
Provide a daily public White House report on how many tests have been done by the CDC, state and local health authorities, and private laboratories.
Expand CDC sentinel surveillance programs and
other surveillance programs so that we can offer
tests not only to those who ask but also to
those who may not know to ask,
especially vulnerable populations like nursing
home patients and people with underlying medical
conditions. This must be done in collaboration
with private sector health care entities.
Task the Centers for Medicare and Medicaid Services to help establish a diagnosis code for COVID-19 on an emergency basis so that surveillance can be done using claims data.
Surge Capacity for Prevention, Response, and
Treatment
Task all relevant federal agencies to take
immediate action to
ensure that America’s hospital capacity can meet
the growing need,
including by:
·
Preparing to stand up multi-hundred-bed
temporary hospitals in any city on short notice
by deploying existing Federal Medical Stations
in the strategic national stockpile and
preemptively defining potential locations for
their use as needed.
·
Directing the U.S. Department of Defense (DOD)
to prepare for potential deployment of military
resources, both the active and reserve
components, and work with governors to prepare
for potential deployment of National Guard
resources, to provide medical facility capacity,
logistical support, and additional medical
personnel if necessary. This includes activating
the Medical Reserve Corps, which consists
of nearly 200,000 volunteer health care
professionals who stand ready to serve across
America; training and deploying additional surge
capacity, including U.S. Department of Veterans
Affairs/DOD medical equipment and U.S.
Department of Health and Human Services (HHS)
Disaster Assistance Medical Teams; and directing
and assisting existing hospitals to surge care
for 20% more patients than current capacity
through flexible staffing, use of telemedicine
support, and delaying elective procedures.
·
Instructing the CDC to establish real-time
dashboards tracking (1)
hospital admissions related to COVID-19,
especially for ICUs and emergency departments,
in concert with the American Hospital
Association and large hospital chains, for which
the HHS must ensure data is able to be shared,
as needed; and (2) supply chain information –
including availability, allocation, and shipping
– for essential equipment and personal
protective equipment, including in the various
places where there may be federal reserves. The
strategic national stockpile must be used to
supplement any shortages that exist, especially
for essential medical supplies, like oxygen,
ventilators, and personal protective equipment.
·
Ensuring that training, materials, and resources
reach federally qualified health centers, rural
health clinics, and safety-net hospitals, which
are typically resource-poor and care
disproportionately for vulnerable populations
that will bear the brunt of COVID-19. This
effort will lay the foundation for a deeper and
more lasting public health infrastructure for
accessible national health care for all.
Surge tele-emergency room, tele-ICU care, and
telemedicine through a concerted, coordinated
effort by health care providers to enable staff
to manage additional patients and save beds for
the
very sick. Leverage
existing efforts like Project
ECHO to
ensure health professionals have tele-mentoring
and other training resources they need to make
informed decisions.
Support older adults, vulnerable individuals,
and people with disabilities. Ensure
essential home- and community-based services
continue and Centers for Medicare and Medicaid
works to provide the waivers necessary for those
who rely on medication to have a sufficient
supply.
Protect health care workers, first responders,
assisted living staff, and other frontline
workers.
·
Give all frontline workers high-quality and
appropriate personal protective equipment – and
enough of it and appropriate training to use it
– so they don’t become infected. If our health
care workers, first responders, and essential
workers like transportation and food workers
cannot function, we cannot protect and care for
the public. The Biden Plan calls for issuing
guidance to states and localities to ensure
first responders and public health officials are
prioritized to receive protective personal
equipment and launching an education campaign to
inform the general public about equipment that
should be reserved for professionals.
·
Direct the Occupational Safety and Health
Administration (OSHA) to keep frontline workers
safe by issuing an Emergency Temporary Standard
that requires health care facilities to
implement comprehensive infectious disease
exposure control plans; increasing the number of
OSHA investigators to improve oversight; and
working closely with state occupational safety
and health agencies and state and local
governments, and the unions that represent their
employees, to ensure comprehensive protections
for frontline workers.
Ensure first responders, including local fire
departments and Emergency Medical Services, can
meet the staffing requirements needed to respond
and are trained to recognize the symptoms of
COVID-19.
Accelerate the Development of Treatment and
Vaccines
Ensure the National Institutes of Health (NIH)
and the Biomedical Advanced Research and
Development Authority are swiftly accelerating
the development of rapid diagnostic tests,
therapeutics and medicines, and vaccines. NIH
must be responsible for the clinical trial
networks and work closely with the U.S. Food and
Drug Administration (FDA) on trial approvals.
Ensure the FDA is working with the NIH to
prioritize review and
authorization for use of COVID-19
countermeasures and strengthen regulatory
science at the FDA to make certain it has the
needed resources to evaluate the safety and
efficacy of new tools.
Provide Timely Information and Medical Advice and Guidance
Work with the CDC and HHS to ensure that health departments and health providers across the country give every person access to an advice line or interactive online advice so they can make an informed decision about whether to seek care or to stay at home. This will preserve the health care system for those who are sick and prevent people who may not need to see a provider from becoming needlessly exposed. Ensure all information provided to the public is accessible to people with disabilities, including through plain language materials and American sign language interpreters.
Instruct the CDC to provide clear, stepwise
guidance and resources about both containment
and mitigation for local school districts,
health care facilities, higher education and
school administrators, and the general public. Right
now, there is little clarity for these groups
about when to move toward social distancing
measures, like cancelling school, mass
gatherings, and travel and when to move to tele-work
and distance learning models.
Ensure firefighters and other emergency responders are notified if they have been exposed to individuals infected with COVID-19.
Launching Urgent Public Health System Improvements for Now and the Future
Work with businesses to expand production of personal protective equipment, including masks and gloves, and additional products such as bleach and alcohol-based hand sanitizer. Incentivize greater supplier production of these critically important medically supplies, including committing, if necessary, to large scale volume purchasing and removing all relevant trade barriers to their acquisition.
Task the U.S. Department of Justice with
combating price gouging for critical supplies.
Take steps in the aftermath of the crisis to produce American-sourced and manufactured pharmaceutical and medical supply products in order to reduce our dependence on foreign sources that are unreliable in times of crisis. The U.S. government should immediately work with the private sector to map critical health care supplies; identify their points of origin; examine the supply chain process; and create a strategic plan to build redundancies and domestic capacity. The goal is to develop the next generation of biomedical research and manufacturing excellence, bring back U.S. manufacturing of medical products we depend on, and ensure we are not vulnerable to supply chain disruptions, whether from another pandemic, or because of political or trade disputes.
Establish and fund a U.S. Public Health Service Reserve Corps to activate former Public Health Service Commissioned Corps officers to expand medical and public health capacity. By creating the Reserve Corps, we will have a larger team of health professionals to deploy across the nation to help train health care systems in detection and response, educate the public, provide direct patient care as needed, and support the public health infrastructure in communities that are often under-resourced and struggling.
Expand the Staffing for the Adequate Fire and
Emergency Response (SAFER) Grant program so that
fire departments – critical first responders in
health emergencies—can
increase staffing. As Vice President, Biden secured an
expansion of the SAFER Act to keep more
firefighters on the job during the Great
Recession. He will expand the grants to build
well-staffed, well-trained fire departments
across the country.
Providing the Resources Necessary to Achieve
These Outcomes
To implement this national emergency response,
the Biden Plan calls
for an immediate increase of federal resources
to cover all necessary federal costs, as well as
the creation of a State and Local Emergency Fund
that gives state and local leaders the power to
meet critical health and economic needs to
combat this crisis. This Fund will be designed
as follows:
Resources will be allocated according to a
formula: 45% to state governments; 45% to local
governments; and 10% reserved for special
assistance for “hot-spots” of community spread.
Menus of Permissible Usages: Governors and
mayors will be given significant flexibility to
ensure that they can target their health and
economic spending where it is most needed in
their respective states and cities. Such usages
include:
·
Paying for medical supplies and expanding
critical health infrastructure, including
building new or renovating existing facilities,
if necessary;
·
Expanding hiring where needed including health
care and emergency services workers, caregivers
in nursing homes, drivers, childcare workers,
substitute teachers, and others;
·
Providing overtime reimbursements for health
workers, first responders, and other essential
workers.
· The Fund will also be deployed to cushion the wider economic impact of the crisis, helping hard-hit families and communities, as described later in the fact sheet.
Bringing Our Country Together
·
Now is the time for empathy, decency, and unity.
In times of crisis, Americans come together, and
everyone steps up to meet our shared civic duty.
We need that spirit now: volunteers standing
ready to fill essential gaps, neighbors looking
out for neighbors, business taking care of their
workers, people contributing to frontline
non-profit organizations, social media companies
combating the spread of misinformation,
universities and the private sector driving
innovation in the search for new treatments and
vaccines, and all of us following the guidance
of health officials to take steps that reduce
the spread of the virus. Biden believes this
can’t just be a government response — it has to
be a whole-of-society response.
ELIMINATING COST BARRIERS FOR PREVENTION OF AND
CARE FOR COVID-19
· The cost of preventive care, treatment, and a potential vaccine could be an insurmountable economic barrier for many Americans. If we fail to remove this barrier, we will be turning our backs on these Americans in a time of crisis, and putting all Americans at risk by discouraging people from getting necessary testing and treatment.
The Biden Plan:
·
Ensures that every person, whether insured or
uninsured, will not have to pay a dollar
out-of-pocket for visits related to COVID-19
testing, treatment, preventative services, and
any eventual vaccine. No co-payments, no
deductibles, and no surprise medical billing. This
will be achieved by:
·
Amending the Public Health Service Act to
immediately cover all testing, treatment, and
preventive services that are necessary to
address a Public Health Emergency for an
infectious disease. Once
triggered by the HHS Secretary in consultation
with the CDC, all commercial plans in all
markets will be immediately required to cover
such services as COVID-19 testing and any
eventual vaccine with no copayments and
deductibles, including for the visits
themselves.
·
Amending the Social Security Act and other
authorizing statutes to extend the same
requirement to all public health programs.
As such, there will be no co-pays for programs
including but not limited to Medicare, Medicaid
and CHIP, the Indian Health Service, the Dept.
of Veterans Affairs, DoD’s TriCare program and
the Federal Employees Health Benefit Plan.
·
Fully funding and expanding authority for the
National Disaster Medical System (NDMS) to
reimburse health care providers for
COVID-19-related treatment costs not directly
covered by health insurance; this includes all
copayments and deductibles for the insured as
well as uncompensated care burdens incurred by
uninsured and underinsured populations. Direct
the HHS Secretary to direct NDMS, in
collaboration with the Centers for Medicare and
Medicaid Services for administrative and
enforcement support, to directly reimburse
health care providers for:
o
All uncompensated care associated with the
testing, treatment, and vaccines that are
associated with COVID-19 for uninsured. This
includes Americans in so-called “junk” health
plans that are not regulated as compliant with
the standards for individual market coverage
under the Affordable Care Act.
o
All copayments, deductibles and any cost-sharing
for treatment for COVID-19 for
insured. Providers will submit
cost-sharing
claims to NDMS that document private insurance
contractual arrangement for co-payments. To
ensure maximum provider participation and
minimum billing abuses to consumers, current
Medicare law’s “conditions of participation” and
system-wide prohibitions against balance billing
and surprise medical bills will apply. To guard
against fraud and abuse by bad-apple health care
providers, harsh civil and monetary penalties
under the False Claims Act will apply.
Secures maximum Medicaid enrollment for currently eligible populations by explicitly authorizing federal matching dollars for presumptive eligibility, simplified application processes, and eligibility criteria. In past public health crises, such as Hurricane Katrina and 9/11, the federal government provided matching dollars for states to expedite enrollment for individuals who are eligible for Medicaid but not yet enrolled. This option must be specifically made available to states for the COVID-19 public health crisis. These policies are consistent with and complementary to the FMAP policy included in the federal economic assistance package below.
Reverses the Trump Administration public charge rule, which places new, burdensome restrictions on documented immigrants who receive public benefits and discourages all immigrants from seeking health care services for COVID-19.
Supports bipartisan efforts to delay the
Medicaid Fiscal Accountability Regulation,
which forces states to change how they finance
their Medicaid programs and leads to major
reductions in funding for critically important
health care.
Additional details are found at
https://joebiden.com/covid-plan/
