
Coronavirus
Technology Solutions
October 21, 2020
Can Foss Fibers with Sciessent Antimicrobials
Inactivate Virus in Transient Droplets?
Masks for Five Billion People Who Cannot Afford
$100/yr
Avery Dennison uses Adhesives to Insure Tight
Fit for Masks
Vogmask has an Efficient, Comfortable Tight
Fitting Mask
Transmission from Surfaces is Far Less than from the Air and Efforts are Being Misplaced
______________________________________________________________________________
Can Foss Fibers with Sciessent Antimicrobials
Inactivate Virus in Transient Droplets?
This was the question posed to Bill Cummings of
Foss and Jeff Trogolo of Sciessent in a
telephone discussion yesterday. It follows an
article we wrote in the October 13 Alert.
In the telephone call we pursued the
potential for ions to move through a transient
droplet and inactivate virus which might
subsequently be released.
The mechanism was described in the
October 13 Alert.
The question is how far the ions will travel
within the droplet. If it is a 10 micron droplet
will there be inactivation on the periphery 180
degrees from the point of contact? Jeff pointed
out that time is also a factor. A large droplet
takes longer to evaporate, so there is more time
for the ions to work their magic.
If, in fact, virus released from small droplets
formed from
large droplets represent a significant
portion of the total and if the viruses can be
inactivated during the large droplet stay on the
mask, then this procedure is quite important.
Search results for: Sciessent
5 results found.
Sorted by relevance / Sort
by date
1. McIlvaine
Coronavirus Market Alert
... Solutions
October 13, 2020 Can Antimicrobials Penetrate
Droplets and Inactivate Virus? Nextera, Sciessent,
and Foss Partner to Produce Antimicrobial Masks Sciessent Antimicrobial
in Nextera Mask Spectrashield Meets ...
Terms matched: 1 - Score: 61 - 14
Oct 2020 - URL:
http://www.mcilvainecompany.com/coronavirus/subscriber/Alerts/2020-10-13/Alert_20201013.html
2. McIlvaine
Coronavirus Market Alert
... Production
from 17 tons per day in March to 51 tons per day
in December Sciessent Antimicrobial
Used in Hanesbrands Masks Teho Filter Using
Ahlstrom Media for N88 Masks in Finland ...
Terms matched: 1 - Score: 50 - 30
May 2020 - URL:
http://www.mcilvainecompany.com/coronavirus/subscriber/Alerts/2020-05-29/Alert_202005029.html
3. McIlvaine
Coronavirus Market Alert
... Coronavirus
Technology Solutions April 21, 2020 Viroblock
Effective Against Coronavirus Sciessent Antimicrobial
in Nextera Mask Spectrashield Meets Efficiency
Requirements Berry Global has New Material for
Surgical Masks NC State ...
Terms matched: 1 - Score: 41 - 29
Apr 2020 - URL:
http://www.mcilvainecompany.com/coronavirus/subscriber/Alerts/2020-04-21/Alert_20200421.html
4. McIlvaine
Coronavirus Market Alert
... Masks
Tustar Teams with Neatrition to Introduce High
Efficiency Masks to the U.S. Market Sciessent Antimicrobial
Used in Hanesbrands Masks Teho Filter Using
Ahlstrom Media for N88 Masks in Finland ...
Terms matched: 1 - Score: 37 - 10
Jun 2020 - URL:
http://www.mcilvainecompany.com/coronavirus/subscriber/Alerts/2020-06-10/Alert_20200610.html
5. Coronavirus
Alerts Table of Contents
... Haul
October 13, 2020 Can Antimicrobials Penetrate
Droplets and Inactivate Virus? Nextera, Sciessent,
and Foss Partner to Produce Antimicrobial Masks Sciessent Antimicrobial
in Nextera Mask Spectrashield Meets ...
Terms matched: 1 - Score: 25 - 20
Oct 2020 - URL:
http://www.mcilvainecompany.com/coronavirus/subscriber/Alerts/TofC.html
Another important use of the technology is to
extend the life of masks.
The fibers can inactivate virus on the
mask surface. This reduces the frequency
of cleaning.
It is particularly important if
comfortable highly efficient and tight fitting
masks are used. If a $30 mask can be worn 100
times the cost is only 30 cents per wearing. If
500 million people spend $100/yr the cost would
be $50 billion worldwide. Fifty million
Americans would spend $5 billion per year. Larry
Summers, former U.S. secretary and Harvard
economics professor estimates that the pandemic
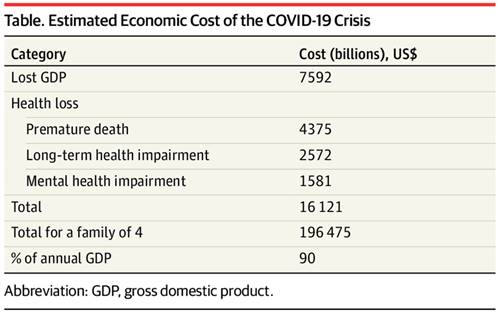
will cost over $16 trillion just in the U.S.
https://jamanetwork.com/journals/jama/fullarticle/2771764
McIlvaine has added the life quality benefits
and costs to the economic costs. The thrill of
attending a motor cycle or political rally is
weighed against the pain of watching loved ones
suffer or even die. This results in an
additional social cost which is greater than the
economic cost.
The fact that masks can be comfortable or even
attractive is part of the calculation of social
cost . Hoodies have been determined by virtue of
teenage expenditures to have life quality
benefits which exceed the discomfort of wear in
the summer time.
Masks for Five Billion People Who Cannot Afford
$100/yr
For those who can only afford $10/yr for masks,
why not buy a $30 mask and wear it for three
years? It will provide far more protection than
the typical cloth mask which is replaced
frequently. If the mask has anti microbials and
can be occasionally cleaned and if it does not
rely on electrostatic charges for efficiency
then this can be the answer for even the poorest
citizens in Asia and Africa. In fact many of the
poorest people are walking around with Michael
Jordan T shirts why not with sterilized used
masks.
Avery Dennison uses Adhesives to Insure Tight
Fit for Masks
Neal Carty, business director, North America,
and senior director, global R&D, Avery
Dennison Medical,
describes the role of skin-friendly adhesive in
a new type of N95 Filtering Facepiece Respirator
(FFR).
None of the “Ps” in Personal Protective
Equipment (PPE) are supposed to stand for
“pain,” but unfortunately that is exactly what
some N95 FFRs are causing for many healthcare
professionals. Nurses, physicians and other
providers have reported rashes and other skin
trauma following long wear times in
tight-fitting N95 half-mask FFRs.
As the medical device industry responds to PPE
requirements, and healthcare institutions look
to build up better stockpiles, new approaches to
FFRs promise to offer clinicians greater choice
and comfort. One such development is an N95 FFR
that adheres directly to the user’s face. This
design eliminates the need for elastic bands to
pull the device against the face. Instead, the
respirator conforms to the face of each
individual end user, secured around the nose and
mouth with a skin-friendly adhesive.

This type of N95 FFR, developed by Global Safety
First and produced and distributed to the
healthcare industry by Avery Dennison Medical,
secures to the wearer’s face with a
skin-friendly acrylic adhesive. Avery Dennison
Medical ©
For any N95 FFR to properly protect the wearer,
there can be no leakage around the edge of the
respirator. To be certified by the National
Institute for Occupational Safety and Health
(NIOSH), these respirators must be proven to
offer protection from particulate materials,
including common bacteria and submicron
particles, with at least 95 percent efficiency.
For a self-adhesive N95 FFR, it is critical for
the adhesive system to provide an effective seal
boundary. The right double-coated adhesive tape
enables this seal integrity. One side of the
tape carries an aggressive adhesive designed to
irreversibly bond to the FFR filtering material,
typically a polypropylene Spunbond Meltblown
Spunbond (SMS) nonwoven. The other side carries
a gentle adhesive designed to adhere the FFR to
the wearer’s skin, where it can remain
comfortably and securely in place for several
hours, if needed.
Of course, with PPE, what goes on must come off.
When the user is finished with the FFR, he or
she must be able to remove it easily, with
minimal discomfort. The skin-facing adhesive
used in the FFR must offer gentle peel adhesion
for atraumatic removal.
In conclusion, the medical device industry is
working to offer healthcare professionals better
PPE options. Skin-friendly adhesives play a key
role in half-mask N95 FFRs that create a
gentle-but-secure protective boundary on the
user’s face.
Vogmask has an Efficient, Comfortable Tight
Fitting Mask
Vogmask has been a leader in masks for air
pollution, wild fires and pollen protection .
McIlvaine contends that masks designed for this
set of contaminants are better suited to the
COVID battle than cloth or surgical masks
The virus is now shown to travel as small
aerosols. It can also attach itself to small
particles.
Keep in mind that the average person
inhales 7.5 million particles as small as 0.1
microns every minute.
Yes, this is every minute not every year.
This is assuming relatively clean air which has
been designated ISO 9. In Mumbai on a bad day or
California when wildfires are burning the
numbers will be much higher. The 0.1 particles
are invisible unless you catch a shaft of
sunlight through your window.
Perfume is mostly particles less than 0.3
microns. So you smell but don’t see it.
Cigarette smoke ranges from 0.1 microns to over
1 micron so some of it is visible but most is
not. This discussion of particle sizes leads to
a conclusion that if you have a mask which does
not protect you from perfume or cigarette smoke
it is not likely to protect you from COVID.
Vogmask has five different sizes and various
other features to provide the tight fit which is
crucial. It has a highly efficient particulate
filter and is comfortable.

The VM filter media in Vogmask has an
obsolescence date three years from manufacture.
Once the middle layer particle filter is
saturated with microscopic particles, there is a
noticeable increase in breathing resistance and
the mask should be replaced. Only in very poor
quality or in proximity to wildfire or other
natural disaster is this likely to occur in as
little as three to five months.
If any part or assembly of the mask is damaged,
or if a good seal is not achievable, discard the
mask. Most Vogmask users replace the Vogmask at
one year of use.
DAILY MAINTENANCE
You may use alcohol wipes >61% or alcohol spray
on surfaces.
Expose to sunlight.
Hand washing: Do not wash the mask frequently.
Excessive washing will eventually affect
filtering efficiency. Do not submerge the
mask. Hand wash rinsing outer and inner layer
with warm water. Add a drop of liquid soap and
gently rub inner and outer layer. Rinse again
and hang to fully dry before storage.
The need to disinfect or clean masks is a
function of the viral load probabilities. If you
are a nurse in a COVID ward the probability is
100% every hour. If you are walking in the woods
with only occasional people passing by the odds
are probably a thousand times less than for the
COVID nurse.
If you are riding the subway in a neighborhood
with a 10% or greater positivity ratio you
probably want to use the alcohol spray or just
rotate masks.
The central thesis in this Alert is that we need
tight fitting efficient and comfortable masks.
The cost is insignificant compared to the
benefits.
Unfortunately few citizens understand the
risks they are taking with loose fitting
inefficient masks. This has to change and when
it does the filtration industry has to be
prepared to meet the needs.
Transmission from Surfaces is Far Less than from
the Air and Efforts are Being Misplaced.
People walking around in cloth masks are
spraying everything in sight but remain at high
risk.
The public over estimates surface risk
and underestimates the airborne risk.
Wired
just had a good summary of what is known about
surface transmission.
A
study on
fomites and Covid-19,
was
released as a preprint in March by researchers
at the University of California, Los Angeles,
the National Institutes of Health, and
Princeton. It was a look at how long the novel
coronavirus lasted on different kinds of
surfaces. At the time, little was known about
how the virus was transmitted, so the question
was important. Depending on the material, the
researchers could still detect the virus after a
few hours on cardboard, and after several days
on plastic and steel. They were careful to say
that their findings only went as far as that.
They were reporting how quickly the virus
decayed in a laboratory setting, not whether it
could still infect a person or was even a likely
mode of transmission.
But in the hazy panic of the time, many people
had already taken up fastidious habits:
quarantining packages at the door, bleaching
boxes of cereal brought back from the store,
wearing hospital booties outdoors. A single set
of research results didn’t start those
behaviors, but—along with other early studies
finding the virus on surfaces in hospital rooms
and on cruise ships—it appeared to provide
validation.
Since March, additional studies have painted a
picture that is much more subtle and less scary.
But like that first study, each can be easily
misinterpreted in isolation. One clear takeaway
is that, given an adequate initial dose, some
amount of the virus can linger for days or even
weeks on some surfaces, like glass and plastic,
in controlled lab conditions. Emphasis on controlled. For
example, earlier this month, an Australian
study published
in Virology
Journal found
traces of the virus on plastic banknotes and
glass 28 days after exposure. The reaction to
that number felt to some like a replay of March:
a single study with a bombshell statistic
sparked new fears about touchscreens and cash.
“To be honest, I thought that we had moved on
from this,” says Anne Wyllie, a microbiologist
at Yale University.
Of course, this was another laboratory study
done with specific intentions. The study was
done in the dark, because sunlight is known to
quickly deactivate the virus, and it involved
maintaining cool, favorable temperatures. Debbie
Eagles, a researcher at Australia’s national
science agency who coauthored the research, says
that taking away those environmental variables
allows researchers to better isolate the effect
of individual factors, like temperature, on
stability. “In most ‘real-world’ situations, we
would expect survival time to be less than in
controlled laboratory settings,” Eagles writes
in an email. She advises handwashing and
cleaning “high-touch” surfaces.
The second consistent finding is that there’s
plenty of evidence of the virus on surfaces in
places where infected people have recently been.
Wherever there has recently been an outbreak,
and in places where people are asked to
quarantine or are treated for Covid-19, “there’s
viral RNA everywhere,” says Chris Mason, a
professor at Weill Cornell Medicine. That makes
going out and swabbing a useful tool for keeping
track of where the virus is spreading.
It’s tempting to piece those two elements
together: If the virus is on the surfaces around
us, and it also lasts for a long time in lab
settings, naturally we should vigorously
disinfect. But that doesn’t necessarily reflect
what’s happening. In a
study published in
September in Clinical Microbiology and
Infection, researchers in Israel tried to
piece it all together. They conducted lab
studies, leaving samples out for days on various
surfaces, and found they could culture the
remaining virus in tissue. In other words, it
remained infectious. Then they gathered samples
from highly contaminated environments: Covid-19
isolation wards at a hospital, and at a hotel
used for people in quarantine. The virus was
abundant. But when they tried to culture those
real-world samples, none were infectious. Later
that month, researchers at an Italian hospital reported
similar conclusions in The
Lancet.
In addition to environmental conditions, a
confounding factor might be saliva, or the stuff
that we often mean when we talk about droplets
sticking onto surfaces. In her own research,
Wyllie has studied how long certain viral
proteins remain intact in saliva to help
determine the reliability of Covid-19 spit
tests. For her purposes, stability is a good
thing. But some proteins have appeared to
denature more quickly than others, she notes,
suggesting the virus as a whole does not remain
intact and infectious. That could be because
saliva tends to be less hospitable to pathogens
than the synthetic substances or blood serums
often used in lab-based stability studies.
Consider, Wyllie says, the extraordinary chain
of events that would need to happen to
successfully spread SARS-CoV-2 on a surface. A
sufficiently large amount of the virus would
need to be sprayed by an infected person onto a
surface. The surface would need to be the right
kind of material, exposed to the right levels of
light, temperature, and humidity so that the
virus does not quickly degrade. Then the virus
would need to be picked up—which you would most
likely do with your hands. But the virus is
vulnerable there. (“Enveloped” viruses like
SARS-CoV-2 do not fare well on porous surfaces
like skin and clothing.) And then it needs to
find a way inside you—usually through your nose
or your eye—in a concentration big enough to get
past your mucosal defenses and establish itself
in your cells. The risk, Wyllie concludes,
is low. “I’ve not once washed my groceries or
disinfected my bags or even thought twice about
my mail,” she says.
Low risk is not, of course, no risk, she adds.
There are high-touch objects that merit
disinfection, and places like hospitals need
clean rooms and furniture. People at high risk
from Covid-19 may want to take extra
precautions. But the best advice for breaking
that object-to-nose chain, according to all the
health experts I spoke with: Wash your hands.
