
Coronavirus
Technology Solutions
October 12, 2020
The Value of Tight Fitting Effective Masks
Demonstrated by White House Events
Mask Fit is Critical to Success Against COVID
But Most Are Not Aware of This
Glendale Arizona Buying Room Air Purifiers with
HEPA Filters
NYC Indoor Restaurants Reopen with HEPA Filters,
UV and Ionizers
Meat Packers Need Efficient Masks and Fan Filter
Units
________________________________________________________________________
The Value of Tight Fitting Effective Masks
Demonstrated by White House Events
On October 10 there was a rally in the Rose
Garden of the White House. An earlier event
celebrating the Supreme Court nomination will
likely result in 100 new coronavirus infections.
This includes the original 13 directly tied to
the event and then others who will be infected
later by the super spreading. The October 10
event will probably result in 200 infections.
Here is why.
|
Parameters |
Supreme Court Event |
Oct 10 Event |
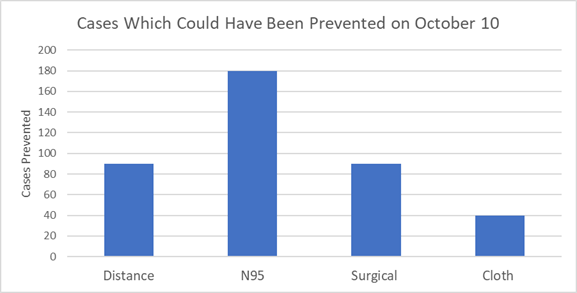
Cases Prevented if Implemented |
|
# of people in attendance |
100 |
400 |
200 Total Preventable |
|
Long Distance Travel |
Yes |
Yes |
|
|
Social Distancing |
No |
No |
90 |
|
N95 Masks |
No |
No |
180 |
|
Surgical Masks |
No |
|
90 |
|
Cloth Masks |
No |
|
40 |
Many of the people traveled by air to the event.
There was no social distancing. Some people were
unmasked but many had cloth masks. Even if some
were wearing surgical masks they were probably
loose fitting. If everyone had been wearing
efficient tight fitting masks, there may be only
20 cases resulting from the event of which only
four would be directly from the event. If
everyone had been wearing surgical masks with
some effort at obtaining a good fit the cases
would be reduced to 110 and 90 deaths prevented.

If everyone had had a loose fitting cloth mask
probably only 40 cases would have been avoided
and there would still be 160.
This
type of behavior is why as of today the
U.S. has had 8 million cases and 220,000 deaths.
The latest models show that we are headed toward
400,000 deaths by January 1. These additional
180,000 deaths could be reduced by 80% with
proper use of tight fitting N95 masks.
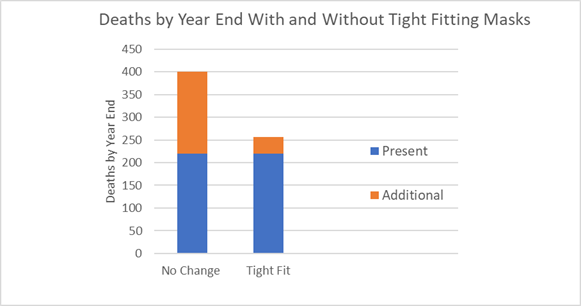
The net benefit to U.S. citizens including both
economic and quality of life will be 180,000 x
$20 million = $3.6 trillion.
This is a net benefit from which an
expenditure of $12 billion for highly efficient
masks is already deducted.
Mask Fit is Critical to Success Against COVID
But Most Are Not Aware of This
A new article in Nature addresses many of
the issues on masks which McIlvaine has been
investigating. However, the problem is the lack
of recognition that a 10 micron droplet
impinging on a mask will evaporate or be
converted into small droplets.
In any case the ultimate salts which
contain the virus will be just a small fraction
of a micron in size. Much of previous mask
efficiency analysis was focused on particles. A
2 micron particle adhering on a mask fiber will
stay there. A droplet will evaporate. So we have
two different situations. Keep in mind that the
sub-micron aerosols or particles will penetrate
in the same way as perfume or smoke.
McIlvaine comments are included in
italics where the information is either
misleading or questionable.
Even well-fitting N95 respirators fall slightly
short of their 95% rating in real-world use,
actually filtering out around 90% of incoming
aerosols down to 0.3 µm. And, according to
unpublished research, N95 masks that don’t have
exhalation valves — which expel unfiltered
exhaled air — block a similar proportion of
outgoing aerosols. Much less is known about
surgical and cloth masks, says Kevin Fennelly, a
pulmonologist at the US National Heart, Lung,
and Blood Institute in Bethesda, Maryland.
In a review of observational studies, an
international research team estimates that
surgical and comparable cloth masks are 67%
effective in protecting the wearer. This may
be true for 5 micron particles but not 5 micron
droplets which become aerosolized. See the mask
leakage vs particle size in the October 9 Alert.
In unpublished work, Linsey Marr, an
environmental engineer at Virginia Tech in
Blacksburg, and her colleagues found that even a
cotton T-shirt can block half of inhaled
aerosols and almost 80% of exhaled aerosols
measuring 2 µm across. Once you get to aerosols
of 4–5 µm, almost any fabric can block more than
80% in both directions, she says. Same
answer. Initial blockage is only the first
phase.
Multiple layers of fabric, she adds, are
more effective, and the tighter the weave, the
better. Another study found that masks with
layers of different materials — such as cotton
and silk — could catch aerosols more efficiently
than those made from a single material.
Eric Westman, a clinical researcher at Duke
University School of Medicine in Durham, North
Carolina, co-authored an August study that
demonstrated a method for testing mask
effectiveness. His team used lasers and
smartphone cameras to compare how well different
cloth and surgical face coverings stopped
droplets while a person spoke. “I was reassured
that a lot of the masks we use did work,” he
says, referring to the performance of cloth and
surgical masks. But thin polyester-and-spandex
neck gaiters — stretchable scarves that can be
pulled up over the mouth and nose — seemed to
actually reduce the size of droplets being
released. “That could be worse than wearing
nothing at all,” Westman says.
Some scientists advise not making too much of
the finding, which was based on just one person
talking. Marr and her team were among the
scientists who responded with experiments of
their own, finding that neck gaiters blocked
most large droplets. Marr says she is writing up
her results for publication.
“There’s a lot of information out there, but
it’s confusing to put all the lines of evidence
together,” says Angela Rasmussen, a virologist
at Columbia University’s Mailman School of
Public Health in New York City. “When it comes
down to it, we still don’t know a lot.”
Questions about masks go beyond biology,
epidemiology and physics. Human behavior is core
to how well masks work in the real world. “I
don’t want someone who is infected in a crowded
area being confident while wearing one of these
cloth coverings,” says Michael Osterholm,
director of the Center for Infectious Disease
Research and Policy at the University of
Minnesota in Minneapolis.
Perhaps fortunately, some evidence
suggests that donning a face mask might drive
the wearer and those around them to adhere
better to other measures, such as social
distancing. The masks remind them of shared
responsibility, perhaps. But that requires that
people wear them.
Across the United States, mask use has held
steady around 50% since late July. This is a
substantial increase from the 20% usage seen in
March and April, according to data from the
Institute for Health Metrics and Evaluation at
the University of Washington in Seattle (see go.nature.com/30n6kxv).
The institute’s models also predicted that, as
of 23 September, increasing US mask use to 95% —
a level observed in Singapore and some other
countries — could save nearly 100,000 lives in
the period up to 1 January 2021.
“There’s a lot more we would like to know,” says
Vos, who contributed to the analysis. “But given
that it is such a simple, low-cost intervention
with potentially such a large impact, who would
not want to use it”
Further confusing the public are controversial
studies and mixed messages. One study in April
found masks to be ineffective but was retracted
in July. Another, published in June, supported
the use of masks before dozens of scientists
wrote a letter attacking its methods (see go.nature.com/3jpvxpt).
The authors are pushing back against calls for a
retraction. Meanwhile, the World Health
Organization (WHO) and the US Centers for
Disease Control and Prevention (CDC) initially
refrained from recommending widespread mask
usage, in part because of some hesitancy about
depleting supplies for health-care workers. In
April, the CDC recommended that masks be worn
when physical distancing isn’t an option; the
WHO followed suit in June.
There’s been a lack of consistency among
political leaders, too. US President Donald
Trump voiced support for masks, but rarely wore
one. He even ridiculed political rival Joe Biden
for consistently using a mask — just days before
Trump himself tested positive for the
coronavirus, on 2 October. Other world leaders,
including the president and prime minister of
Slovakia, Zuzana Čaputová and Igor Matovič,
sported masks early in the pandemic, reportedly
to set an example for their country.
Denmark was one of the last nations to mandate
face masks — requiring their use on public
transport from 22 August. It has maintained
generally good control of the virus through
early stay-at-home orders, testing and contact
tracing. It is also at the forefront of COVID-19
face-mask research, in the form of two large,
randomly controlled trials. A research group in
Denmark enrolled some 6,000 participants, asking
half to use surgical face masks when going to a
workplace. Although the study is completed,
Thomas Benfield, a clinical researcher at the
University of Copenhagen and one of the
principal investigators on the trial, says that
his team is not ready to share any results.
For now, Osterholm, in Minnesota, wears a mask.
Yet he laments the “lack of scientific rigor”
that has so far been brought to the topic. “We
criticize people all the time in the science
world for making statements without any data,”
he says. “We’re doing a lot of the same thing
here.” The emphasis on gathering data rather
than understanding the processes and creating
accurate formulae seems to be a difference
between the medical community and those involved
with aerosol science. Droplet evaporation can be
predicted and there are experts to make the
calculations (see the MIilvaine interview with
the UCSD droplet expert).
This article by Lynne Peeples is found at
https://www.nature.com/articles/d41586-020-02801-8
Glendale Arizona Buying Room Air Purifiers with
HEPA Filters
With in-person learning back among Deer Valley
Unified School District campuses, the district
this week will present on its emergency
acquisition of air purifiers and filters for
campus buildings in ongoing precautionary
efforts against coronavirus.
Director of Finance Heather Mock will submit the
request for a purchase total of $666,547.70 to
procure air purifiers and filters for all
district classrooms.
“Due to Covid-19 epidemic and updated
recommendation from the Maricopa County Public
Health Services – Ventilation in a School
Setting, Districts should use portable room air
purifiers with HEPA filters, especially in
higher-risk areas,” the district wrote of its
emergency incident. “Due to the current demand
for these air purifiers, these items are scarce
and have long-term delivery windows, which are
extending daily.”
“Therefore, due to time constraints and
availability, the district found it in the best
interest to prioritize and place the purchase
prior to the next scheduled governing board
meeting. The purchase was procured through an
approved Cooperative, due diligence was
performed, and quotes were obtained.”
The request states that Grainger provided the
best value and availability.
HEPA, or high efficiency particulate air
filters, “can theoretically remove at least
99.97 percent of dust, pollen, mold, bacteria,
and any airborne particles with a size of 0.3
microns,” according to epa.gov.
The first round of a staggered return to
live learning around the district came on Sept.
24. The final round will see K-8 middle school
grades and high school freshmen return to their
respective campuses on Wednesday, Oct. 14, at
which time all district campuses will be back to
full occupancy with safety guidelines in place.
NYC Indoor Restaurants Reopen with HEPA Filters,
UV and Ionizers
New York City reopened for indoor dining at 25
percent capacity starting on September 30.
There are requirements such as PPE for
the service people.
Top Line Hospitality Services owner Scott Bankey
has been upgrading restaurants’ HVAC units to
MERV-13.
On the roof of the Michelin-starred Musket Room
in Soho, Bankey installed a bit more:
ultraviolet lamps designed to inactivate up
to 99 percent of funguses, bacteria, and
viruses in
the air that’s been vented from the restaurant.
The sanitized air then hits the filter, is mixed
with fresh air, and is pumped back inside.
Musket Room staff were at first anxious about
serving unmasked customers indoors, but owner
Jennifer Vitagliano reviewed the additional
modifications with them so that they could
research it for themselves. “Everyone feels
really confident that we’re going above and
beyond to create a safe environment,” says
Vitagliano, who would not confirm the exact
price of the modifications but said that it cost
the restaurant “a few thousand dollars.”
William Bahnfleth, professor of engineering at
Penn State University, who focuses on HVAC
(heating, ventilation, and air conditioning),
thermal storage, and indoor air quality in his
research. He weighed in on UV.
“There’s a very
good track record for
UV, because it’s been used in infection control
since at least the 1930s,” says Bahnfleth, who
also serves as the chair of the epidemic task
force for ASHRAE (American Society of Heating,
Refrigerating and Air Conditioning Engineers).
“It wasn’t something that most people were aware
of, but it’s been around for a long time. I’ve
been doing research on it for over 20 years.”
Le Bernardin, the only three-Michelin-starred
restaurant to reopen September 30 — the first
day indoor dining is allowed again in NYC has
installed a Needlepoint Bi-Polar Ionization
system, which they say is “proven to eradicate
99.4% of airborne COVID-19 particles within 30
minutes.” The technology sounds like the stuff
of science fiction: Charged particles are
released into the air to hunt for dust and
viruses, deactivating them upon contact. While
UV lamps rely on air that’s been sucked into the
HVAC unit to be sanitized, bi-polar ionization
systems are, in theory, proactive. Their
efficacy is still up for debate, since there
have been few peer-reviewed studies on the
technology.
“What ionizers definitely do is charge particles
so that they stick together and they can be
removed from the air more efficiently,” says
Bahnfleth. “Like UV, ionizers have been around
under the radar for quite a while, but they’re
just something everyone’s aware of now because
of the pandemic. They weren’t invented
yesterday.”
The cost of these units is high, especially for
restaurants that are already financially
strapped as a result of the pandemic. The team
at Crown Shy in the Financial District is
operating at just 10 percent of their
pre-pandemic revenue but spent $40,000 adding a
bi-polar ionization system to the HVAC units
that service both the ground-floor restaurant
and its soon-to-open restaurant
in the sky,
Saga.
“It’s expensive, but it’s worthwhile,” says
general manager and partner Jeff Katz. “Our
first concern is making people feel comfortable
in the space, so that they can think as little
as possible about the global pandemic. Nothing
ruins a meal like the thought of pathogens.”
AtmosAir, which manufactures the units that were
installed in Crown Shy, has seen its revenues
rocket to five to six times what it was at this
point last year. “Demand is very high in New
York City,” says Brian Levine, AtmosAir’s vice
president of marketing.
Coronavirus preparation, like most other things,
is a battle between the haves and have nots.
Smaller neighborhood joints are more likely to
just buy HEPA air filter units for several
hundred dollars. But an organization like Union
Square Hospitality Group, which operates
restaurants like Gramercy Tavern, Blue Smoke,
and Union Square Cafe, can afford to leave no
box unchecked, spending tens of thousands of
dollars to beef up its filtration systems,
adding both a UV light rig and bi-polar ionizer
at each of its locations.
While these extra precautions may be helpful to
ease the minds of a shell-shocked population,
the state reopening guidelines also recommends
simple things like a basic ventilation system or
even leaving all the doors and windows open.
Restaurants in the Northeast and the rest of New
York State have been open for indoor dining for
months without a surge in coronavirus cases,
despite many places lacking the resources to
install high-end HVAC systems.
In recent interviews,
the nation’s leading infectious disease expert,
Dr. Anthony Fauci, stated that dining indoors
“absolutely increases the risk,” but stressed
the importance of harm reduction in dealing with
COVID-19. “There comes a point where you’ve got
to accept human nature,” Fauci said of people’s
desire to socialize. He added that in addition
to a low local positivity rate, “anything that
has airflow out, not airflow in the room” was
the key to making restaurants safer.
“There’s a lot of evidence that good ventilation
is protective,” says Bahnfleth. “And when you
add filters to it and air cleaners, things get
even better.”
https://ny.eater.com/2020/9/30/21494934/nyc-restaurants-indoor-dining-air-filters-cost-coronavirus
Meat Packers Need Efficient Masks and Fan Filter
Units
There is an extensive analysis of the meat
packing industry attempts to protect workers in
Mother Jones by Tom Philpott.
He is the food and ag correspondent for Mother
Jones. He can be reached at
tphilpott@motherjones.com, or on Twitter at
@tomphilpott.
We are showing the Philpott analysis with our
comments in italics. The coronavirus has fallen
heavily on the people who cut and pack the US
meat supply. After blitzing meatpacking plants
all spring and summer, the illness has infected
at least 43,100 of these workers and killed 206,
according to the running tally kept by the Food
and Environment Reporting Network’s Leah
Douglas. Lately, new cases and deaths within the
industry have been leveling off, according to
Douglas’ data. And media attention has shifted
from the deadly toll on workers to the gentle
penalties the Trump administration has imposed
on the massive companies that dominate the meat
industry for their worker-safety performance
during the crisis.
Though it’s failed to garner much national
attention, the deadliest meatpacking outbreak of
all has unfolded in recent weeks in California’s
agriculture-dominated San Joaquin Valley. On
September 1, West Coast poultry powerhouse
Foster Farms closed its Livingston, California,
chicken plant by order of the Merced County
Department of Public Health,
after acknowledging 392 positive COVID-19 tests
and eight deaths among employees. After another
plant employee who had been hospitalized with
COVID since August died in mid-September, the
outbreak’s death toll now stands at nine, the
most COVID-related fatalities of any single
meatpacking plant, according to FERN’s Douglas.
Could the company have done more to prevent the
outbreak? The Merced County health department
repeatedly warned Foster Farms to ramp up
efforts to protect its employees, before any
deaths occurred. In an August 27 press
release, the health department reported that it
had been unsuccessfully urging Foster Farms to
take precautionary safety measures since late
June, a “month prior” to any COVID-related
deaths.
On June 29, as COVID cases at the plant
“continued to rise,” county health officials
inspected the plant. To limit the outbreak, the
health department suggested “significant changes
to the employee break spaces and performing
widespread testing of employees within the
facility.” The department continued to call for
a testing ramp-up throughout the month of July,
but by the final days of the month, Foster Farms
had “tested less than 10 percent of the
department with the largest [COVID] impact
within the facility,” the report states. Among
the employees who were tested, more than 25
percent turned up positive.
In August, the department stepped up its
campaign to push Foster Farms to increase
testing and tweak common areas. On August 3,
officials made a second visit to the Foster
plant—this time accompanied by representatives
of Cal/OSHA, the state’s worker-safety
enforcement agency. On August 5 and 11, the
department repeated its call on the company to
increase employee testing and tweak common areas
to enable social distancing. Meanwhile, the
coronavirus continued to spread through the
complex, “posing a significant threat to Foster
Farms employees and the surrounding community,”
the health department report states. Finally, on
August 27, two months after its initial call for
common-area changes and widespread testing, the
health department ordered the plant to
close, pending universal employee testing and
“significant changes” to all break spaces and
“areas of potential congregation” to “ensure
adequate social distancing of all workers on the
plant.” In the period of time between the
initial June 29 recommendations and the August
27 close order, eight workers died of COVID-19.
The company failed to keep workers informed
about the outbreak as it spread through the
plant over the summer, says Erika Navarrete of
the United Farm Workers of America, which
represents the plant’s workers. Workers have
told Navarrete that Foster Farms has only given
them two masks per person total since the start
of the pandemic, so they’ve had to buy this
crucial protection themselves. And while the
company has installed plexiglass barriers
between stations on the facility floor, “workers
are still too close together,” working
shoulder-shoulder on the line, says Navarrete,
who has visited the plant several times. A
Foster Farms spokesperson declined to comment.
The conditions described by Navarrete—masked
workers toiling close together, separated by
plastic barriers—appear to be standard
poultry-industry practice during the COVID
crisis. In an article entitled
“Our #1 Priority: Keeping Chicken Company
Employees Safe & Healthy During COVID-19,” the
National Chicken Council—a trade group
representing US chicken processors—includes the
below photograph of workers on a
chicken-production during the pandemic. A
National Chicken Council spokesperson alerted
that meat giant Tyson Foods had posted the photo
on a web gallery available to media showing the
“protective measures” the company is taking in
response to COVID-19.

Is the arrangement sufficient to protect workers
from COVID? Federal worker-safety authorities
are fuzzy on the topic. The US Occupational
Safety and Health Administration has declined to
issue binding workplace regulations to impede
the spread of COVID. Along with the Centers for
Disease Control and Prevention, OSHA released voluntary
meatpacking-industry guidelines on
July 26. The guidelines call on companies to
“modify the alignment of workstations, including
along processing lines, if feasible, so that
workers are at least six feet apart in all
directions (e.g., side-to-side and when facing
one another), when possible.” They also suggest
“physical barriers, such as strip curtains,
plexiglass or similar materials…to separate meat
and poultry processing workers from each other.”
The guidelines don’t comment on whether barriers
negate the need for social distancing.
Two independent occupational health experts
Philpott consulted
say distancing is essential, with or without
barriers in place. “Medical masks and plastic
sheeting are not enough,” said David Michaels,
who served as chief of the Occupational Safety
and Health Administration under President Barack
Obama and is now a professor of environmental
and occupational health at George Washington
University. He pointed to a July 2020
investigation by
German scientists of a COVID-19 outbreak in a
German meatpacking plant which found that
“climate conditions and airflow” in these plants
can “can promote efficient spread” of the virus
at “distances of more than 8 meters,” or 26
feet. “Workers in poultry plants need greater
distance between them, and they need
respirators, not medical masks,” Michaels said.
The important point here is that you need
respirators not masks. Furthermore these
respirators have to be tight fitting. Look at
this picture and
envision that many of the workers are
smoking cigarettes. How effective would the
partitions or loose fitting masks be?
Plastic barriers are “more effective in a
grocery store situation where you’re having very
quick interactions with people,” said Marissa
Baker, director of the Industrial Hygiene
Training program at the University of
Washington’s Department of Environmental &
Occupational Health Sciences. But in meatpacking
plants, “you’re standing shoulder to shoulder
with someone for eight hours a day—unless you’re
in your own separate box, there’s definitely a
chance for virus to get around those barriers.”
She said a safer approach would be to keep the
barriers but spread workers at least six feet
apart—which would likely require the company to
slow down its production. A slower line would
also protect workers from COVID-19 in another
way, Baker added: “When you have people working
fast, people are breathing harder—and that leads
to more particle generation,” and thus more
potential exposure to pathogens.
You could keep the close spacing if you have fan
filter units spaced along the line. The downward
clean air flow will keep the virus from moving
horizontally.
“Medical masks and plastic sheeting are not
enough,” according to occupational safety expert
David Michaels.
When the COVID crisis took root in the spring,
Foster Farms joined several other meatpacking
companies in delivering its workers a salary
bonus of $1 per hour for working
shoulder-to-shoulder during a pandemic. But the
company ended the bonus on May 31—just before
the disease began to spread through the plant,
Navarrete said. UFW is currently negotiating
with Foster Farms on a contract for the plant’s
workers, she added, and is demanding $2 per hour
hazard pay for the duration of the pandemic.
It remains to be seen whether Foster Farms will
face penalties for its management of the
Livingston outbreak. So far, despite widespread
contagion and fatalities in plants across the
country, Trump’s OSHA has doled out two fines—at
levels that Michaels, the former OSHA
administrator, has called “less
than a slap on the wrist.” Trump’s OSHA
recently hit pork
giant Smithfield with a $13,494 fine for an
April outbreak that infected at least 1,294
workers and killed 4 at its massive pork
operation in Sioux Falls, South Dakota; and it
laid a $15,615 penalty on meatpacking behemoth
JBS for
an outbreak that led
to 300
positive tests and six worker deaths at its
Greeley, Colorado, beef plant.
In California, worker-safety laws are enforced
by a state agency called Cal/OSHA, a division of
the California Department of Industrial
Relations. On September 9, Cal/OSHA hit mid-sized
frozen-foods manufacturer, Overhill Farms, with
a $200,000 fine, and levied another $200,000 one
on the temporary-employment agency it uses,
Jobsource North America. Their infraction,
according to the press
release:
They failed to take measures to protect workers
from COVID-19, resulting in “more than 20
illnesses and, in the case of Overhill Farms,
one death.”
On September 8, Foster Farms reopened its
Livingston plant after complying with health
department conditions. Whether
it will pay a price for the outbreak remains to
be seen. In an email, a spokesman for the
California Department of Industrial Relations
wrote: “Cal/OSHA opened an inspection on July 23
at the Foster Farms in Livingston after
notification that a worker died from
complications related to a COVID-19 infection.”
He declined to comment further on what he called
an “ongoing inspection” of the plant, but added
that “by law, Cal/OSHA has up to six months from
the opening date of an inspection to issue
citations.” In the meantime, dozens of workers
in the plant continue to work shoulder to
shoulder as the pandemic grinds on.
