
Coronavirus
Technology Solutions
October 7, 2020
Efficient Tight Fitting Masks are Needed to Beat
COVID
Supreme Court Nomination Celebration was a Super
Spreader Event
Increase the Effectiveness of Standard Face
Masks
Ten to Forty Percent of Particles will Penetrate
a Surgical Mask Due to Poor Fit
Respirators are Much More Protective than
Surgical Masks
Reinfection is Happening but not on a Large
Scale
____________________________________________________________________________
Efficient Tight Fitting Masks are Needed to Beat
COVID
The evidence appearing in the daily alerts in
the Coronavirus Technology Solutions
shows that
·
Most of the transmission is through small
aerosols
·
Large droplets on the mask’s internal surface
become small aerosols
·
The typical surgical mask is only half as
efficient as a tight fitting high efficiency
mask
Small aerosols containing coronavirus are
inhaled and exhaled through the periphery of
surgical masks. The COVID battle will be won
with either N95 masks or improved versions of
surgical masks which minimize leakage.
Tight fitting masks are inherently more
uncomfortable and require more effort to wear
properly than the typical surgical mask. Since
the virus travels as easily as perfume or
cigarette smoke the tighter the fit the better.
There are recent innovations to provide a
tighter fit. One is a self-adhesive mask.
Others add a peripheral band which is
adjustable. This is a solvable problem which
will not add much to cost.
An individual should have multiple mask types
which he wears as conditions warrant.
This can range from N100 down to tight
fitting surgical masks.
It can include non-valved as well as
valved designs.
Much of the time no mask will be required. The
mask selection at any point in time should be
appropriate to the risk in a specific
environment. This risk is indicated by
-
New COVID-19 case counts
-
Incidence rate (new cases per
100,000 people), and
-
New case trajectory (whether the
number of new cases is going up,
going down, or staying the same
over time).
-
Indoor and outdoor pollution
levels
-
Testing Positivity ratios
-
Site specific factors such as
number of people per ft2. Air
changes per hour and efficiency
of HVAC systems
Individuals should continually assess risks and
wear the appropriate mask for the circumstances.
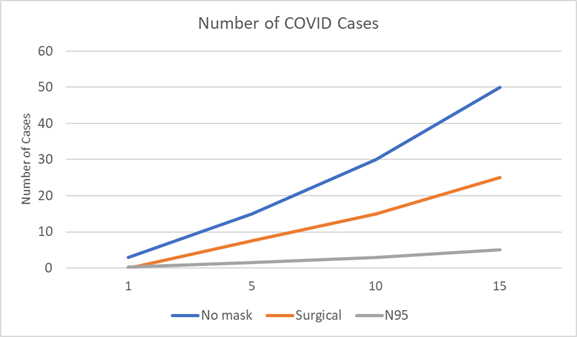
Let’s take an example which
is prominent in the news The cost of
holding the Supreme Court nomination at the
White House in September is estimated at $140
million as a result of
coronavirus cases and deaths which will
result from this one event.
This amount is based on the eventual deaths of
two people and infection of 100 people as
attendees pass the virus along to non-attendees.
Social distancing would have cut the cases to
50. In addition surgical masks would have
reduced the cases by another 25. N95 masks would
likely have reduced the cases to five.
Even with the N95 masks the risk is
unacceptable. When all costs including quality
of life are considered it would have been an $8
million cost for one event. This is much less
than the $140 million actually generated with no
masks or social distancing but still too high a
price to pay.
This event was predictably high risk. One metric
would be to assume a net positive ratio in
excess of 15 as a rating of risk for this event.
There are some parts of the country where the
risk is well less than 1%
if only a small number of local people
attend.
The number of cases of an infection for a
proposed event can be predicted depending on the
risk.
In this case we used net positive rate as
the indicator and compared results for rates of
1 to 15.
McIlvaine has created a methodology to assess
the costs and benefits of various mask
decisions.
This includes healthcare costs, economic
costs and life quality costs. It is then
balanced by the benefits of lives saved and
cases avoided which has both economic and life
quality components.
There is a detailed analysis of these
costs and benefits for the White House event in
the October 7 Coronavirus Technology
Solutions alert.
The costs and benefits of various masks along
with their availability are analyzed in the
High Efficiency Mask Market and Supplier
Program.
Click here to
view a video description or Click
here for
the power point display
Supreme Court Nomination Celebration was a Super
Spreader Event
The Supreme Court Nomination is turning out to
be a super spreader event. This event can be
used as an example of how best to fight the
disease. The event was held partially indoors
and partially in the Rose Garden with closely
placed chairs.
There were therefore the following potential
factors in the extent of the transmission
1.
Number of infected people in attendance
2.
Indoor air filtration efficiency and flow
3.
Outside air wind velocity and direction
4.
Number of people wearing masks
5.
Types of masks worn
6.
Activities of participants
The benefits have to be weighed against the
costs which include both
economic and social. The most extreme
form of social distancing is quarantining with
high life quality costs. If the
Supreme Court nomination ceremony had
been remote, the transmission risk would have
been eliminated. At a minimum keeping a distance
of six feet would be a social distancing tool.
In terms of the social cost of a virtual
ceremony the nominee could very easily traded a
month or oven months of vacation time for the
one Rose Garden event. Most of the attendees
would probably been willing to give up one day
of vacation for the event.
The life quality cost of staying six feet apart
at the ceremony might have been worth trading a
few days of vacation by the nominee but probably
not worth a few hours on a Hawaiian beach for
most attendees.
At this point at least ten people probably
contacted the virus directly at the event. The
fact that each of them is statistically likely
to have infected 20 other people who in turn
will infect 40 people means that the number of
cases and ultimately deaths attributable to the
event will be substantial. Let’s assume that
there will be two deaths and 100 infections as a
result of the event.
At $20 million per death and $1 million
per infection, the economic and life quality
costs will exceed $140 million just from this
one event.
Social distancing, HVAC with efficient air
filters, and masks would have been useful in
minimizing the transmission.
Social distancing: the protocol to keep six foot
distant at all times by itself may have cut the
transmission in half.
No capital cost would have been required.
So
$70 million would have been saved.
But the cost would still be $70 million. Fifty
people would become infected and one would die.
The
virus floats through the air like perfume.
So the air flow and speed both inside and
outside would be a factor.
HVAC:
portable room air purifiers could have
been provided for every 100 ft2 area outside.
fifty air purifiers would have a capital cost of
around $25,000 but the rental for one day might
be only $2,000.
The HVAC in the inside air could have
been upgraded to more than 15 air changes per
hour and HEPA filters. The cost for a large room
might be $40,000 but if it is used continually
the cost could be depreciated over a number of
events. Alternatively the portable air filters
could have been moved inside for that part of
the event. So the cost for this event might be
$4,000. The savings could be 15 cases and
0.25 deaths or $20 million.
Surgical masks:
the effectiveness will only be 50% due to
leaks around the masks. So the additional saving
after social distancing would be 25 cases and
0.5 lives for a saving of
$35 million. The cost for 200 people
wearing a surgical mask during the event would
be $400. Using the vacation time as an example
of social cost the nominee may have been willing
to trade a week’s vacation time for the
event to be free of masks. Most attendees
would be unlikely to trade even a few hours.
N95 Masks: the
effectiveness will be 90%. It would eliminate 45
cases
and 0.9 lives lost.
So the saving is $63 million. The cost
would be $800.
The social cost of the N95 might be a
little higher than for the surgical mask but not
if the N95 is designed for comfort.
|
|
Social
Distancing |
Technologies in
Addition to
Social
Distancing |
||
|
HVAC |
Surgical Mask
|
N95 Mask |
||
|
Lives saved |
1 |
0.25 |
0.5 |
0.9 |
|
Infections
Avoided |
50 |
15 |
25 |
45 |
|
Benefits |
$70 million |
$20 million |
$35 million |
$63 million |
|
Economic cost |
0 |
$4,000 |
$400 |
$800 |
|
Life quality
Costs |
$1 million |
0 |
$10,000 |
$10,000 |
|
Net benefit |
$69 million |
$20 million |
$35 million |
$63 million |
|
Net cost |
$71 million |
$51 million |
$36 million |
$8 million |
Increase the
Effectiveness of Standard Face Masks
Reducing mask leakage will very important. There
is progress being made. One innovation came
after a study by two University of
Wisconsin-Madison mechanical engineering
professors revealed that various existing masks
and face shields allow tiny particles to escape,
both through the material and at the edges. If
the wearer is infected with the novel
coronavirus, that means the virus could travel
from the wearer’s mouth or nose and infect those
around them.
The research came from professors Scott Sanders
and David Rothamer, who usually study combustion
engines and use laser illumination to find the
leaks. Back in April, they turned their
expertise and tools toward solutions to the
growing pandemic.
Over the following months, they conducted
numerous tests of various face coverings,
placing the coverings on mannequins and using a
foggy-looking substance made from salt and air
to simulate the aerosolized particles in human
breath.
In one experiment, they set 17 former CPR
mannequins in a classroom to simulate students
wearing various forms of protective equipment
and pumped the aerosols through them. In another
experiment, they pumped a larger volume of
aerosols through a single mannequin’s mouth and recorded
video of the results.
The video of the mannequin wearing the face
shield shows fog escaping out the bottom, while
the mannequin wearing a loose-fitting surgical
face mask fogged from the top and sides.
For a better seal, the two researchers used
packing tape to attach the masks to the
mannequins’ heads, and the amount of leaking
aerosols fell dramatically.
Knowing that living humans wouldn’t tape their
masks to their faces, they asked Lennon Rodgers,
director of UW-Madison’s Grainger Engineering
Design Innovation Lab, to help devise an
alternative for tightening the fit of a standard
surgical mask.
Rodgers and Sanders soon discovered online that
there were a few products already on the market
for this purpose, known as “mask fitters,” but
none met the goals for the product, Rodgers
said, noting the relative expense of 3D
printing.
“I was thinking this has to be dead simple. It
has to be so cheap,” he said, citing the success
of the original Badger Shield design which used
only three easy-to-find materials and was
soon being produced at a massive scale by
manufacturers around the world.
“My thought was like if we wanted to make tons
and tons of these, like millions, and make it
very cheap, 3D printing is pretty much out the
window.
 ”
”
![]()
The Badger Seal, the latest PPE innovation
released by the UW Makerspace, can be worn over
a surgical or cloth mask to provide a tighter
fit and reduce particle penetration. The design
was dubbed the Badger Seal.
When Sanders and Rothamer tested the Badger Seal
on the mannequins, they now needed lasers to
detect the escaping aerosols that had previously
been visible to the naked eye. The device
increased the filtration efficiency of a
standard surgical mask by three times and
increased the efficiency of a cloth mask by four
to eight times. Those efficiency gains led to
even bigger changes in particle penetration.
When worn over a three-layer disposable mask,
the Badger Seal yielded particle penetration 15
to 18 times less than that of a cloth mask.
Like the team’s other personal protective
equipment designs, the Badger Seal designs are
open-source, which means there's no patent.
People can build their own using instructions
and videos.
Each can be made in about five minutes with
basic tools and materials that cost less than a
dollar, and members of the UW-Madison campus
community can make their own using materials at
the DIY station in the Makerspace lobby.
The university has already built about 2,500
Badger Seals in-house. Some have been
distributed to faculty and custodians, but
plenty are still on hand, Rodgers said.
The research side of the project is likely
complete. “It's more now about kind of getting
the word out there about the various PPE options
people have that they probably don't know
about,” Sanders said, though he’s still running
tests weekly.
Digital Publishing and Printing Services, the
university’s printing service, which pivoted
back in April to make Badger Shields for UW
Health, is now making Badger Seals for campus.
If demand outside campus proves sufficient,
Rodgers said he and his team would find a
manufacturer interested in producing them. But
so far, the new design hasn’t seen the same
interest as the Badger Shield and it’s
extra-protective cousin the Badger Shield Plus,
the latter of which launched
as teachers and students (both K-12 and college)
prepared for a return to
in-person instruction
Ten to Forty Percent of Particles will Penetrate
a Surgical Mask Due to Poor Fit
The filters of most surgical masks will allow a
large majority of wearer-generated particles to
penetrate and will collect only a small
percentage of airborne particles generated by
infectious patients. Even when equipped with
filters demonstrating relatively high collection
efficiency, 10% to 40% of particles will
penetrate the face seal as a result of poor fit.
For aerosols containing organisms with a low
infectious dose (e.g. tuberculosis), this level
of face seal leakage would not prevent a
potentially infectious exposure during even a
brief encounter with a patient generating
copious amounts of aerosol. The poor performance
of dental masks is of particular concern, given
dental surgeons' close proximity to patients and
the high aerosol concentrations generated by
dental procedures.
Respirators are Much More Protective than
Surgical Masks
There are few studies that compare the clinical
efficacy of respirators versus surgical masks.
In one Toronto hospital, all attending health
care workers reported to be wearing
“respirators” contracted severe acute
respiratory syndrome (SARS) during a patient
intubation. Closer examination reveals that
employees were wearing surgical masks, not
respirators. Another study found that nurses in
a Toronto hospital not consistently wearing
either a filtering face-piece N95 respirator or
a surgical mask had four times the risk of
contracting SARS as those consistently wearing
respirators or surgical masks. Fit testing is
not required and was infrequently employed in
Canada during the SARS outbreaks.
Data illustrate how important fit is to
preventing inward leakage of particles.
Qualitative fit tests are considered valid
measures of personal protection for respirators
that must achieve a fit factor of 100 (used in
atmospheres less than 10 times the permissible
exposure limit). Although two subjects were able
to pass the qualitative fit test on two
different surgical masks when assisted with fit,
the authors believe these results occurred
because of temporary taste desensitization.
Quantitative fit test results support this
conclusion. None of the test surgical masks
attained an individual fit factor of 100, the
minimum level expected for a half-mask filtering
face-piece respirator. Assistance with fit made
no difference in the degree of fit.
Qualitative fit test results also illustrate the
importance of surgical mask design. Mask D
showed the second highest filter efficiency but
the lowest fit factor. One of the reasons for
poor fit may be the ear loop design, which
limits adjustability of fit. To be effective in
reducing wearer's exposure to airborne
substances, a respiratory protection device
needs to have sufficient fit as well as high
filtration efficiency
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7115281/
Reinfection is Happening but not on a Large
Scale
On 15 August, a 33-year-old man landed in Hong Kong after flying home from Spain. On arrival, he was screened for coronavirus. Despite feeling well he tested positive. It was the second time he had picked up Covid-19 in less than five months.
The case immediately caught scientists’ attention. The man was the first in the world to have a confirmed coronavirus reinfection and there were positives to take from the report. First and foremost, he was asymptomatic. Although reinfected with Sars-Cov-2, his immune system swung into action fast and contained the virus without him knowing.
Many researchers took heart from the case, but since the patient came to light a flurry of reinfections around the world have raised fresh concerns. Within days of the Hong Kong case being made public, doctors in the US reported that a 25-year-old man from Reno, Nevada, had been hospitalized with a Covid-19 reinfection after shrugging off an earlier brush with the disease. More cases soon followed. While most infections were no worse the second time around, a good number cropped up – in the US, the Netherlands, Ecuador and India – where the reinfection was more severe.
“It’s really hard to find a pattern right now,” said Akiko Iwasaki, a professor of immunobiology at Yale University who has been following cases of reinfection closely. “Essentially every case is different.”
So far, only two dozen or so reinfections have
been confirmed worldwide in a pandemic that has
infected more than 30 million people. For now at
least, reinfection seems uncommon. But
scientists point out that confirming reinfection
is no easy task and many cases are missed.
To confirm a reinfection, scientists must
examine the genetic code of the virus from each
round of illness and prove they are distinct.
That means having access to both sets of swabs
and the wherewithal to do whole genome
sequencing. Even in hospitals where the capacity
exists, such tests are rarely done. Reinfected
patients simply go unnoticed or unreported.
“There is probably a lot more than we are
seeing,” said Iwasaki.
