
Coronavirus
Technology Solutions
October 6, 2020
Evaporation and Breakup of Droplets Included in
Face Mask Study
Study in Israel Concludes that Masks are Used
Improperly
Respirator with HEPA Filter for Both Inhalation
and Exhalation
Slate Magazine
Says Airline Case Studies are not a Worry If
People Wear Masks
BTL N95 Masks Meet All Required Test Protocols
Surgical Mask Leakage is a Major Hurdle to
Besting COVID
_____________________________________________________________________________
Evaporation and Breakup of Droplets Included in
Face Mask Study
Researchers at the University of Nicosia have
added insights on aerosol generation of droplets
from mask surfaces.
Face mask filters—textile, surgical, or
respiratory—are widely used in an effort to
limit the spread of airborne viral infections.
Our understanding of the droplet dynamics around
a face mask filter, including the droplet
containment and leakage from and passing through
the cover, is incomplete. We present a fluid
dynamics study of the transmission of
respiratory droplets through and around a face
mask filter. By employing multiphase
computational fluid dynamics in a fully coupled
Eulerian–Lagrangian framework, we investigate
the droplet dynamics induced by a mild coughing
incident and examine the fluid dynamics
phenomena affecting the mask efficiency. The
model takes into account turbulent dispersion
forces, droplet phase-change, evaporation, and
breakup in addition to the droplet–droplet and
droplet–air interactions. The model mimics real
events by using data, which closely resemble
cough experiments.
The paper does touch on the
potential for drop
penetration but more detail will be
requested. However it does show large droplets
are aerosolized and penetrate the mask.
Others rebound
and in the case of surgical masks or cloth masks
can then escape through the openings around the
mask.
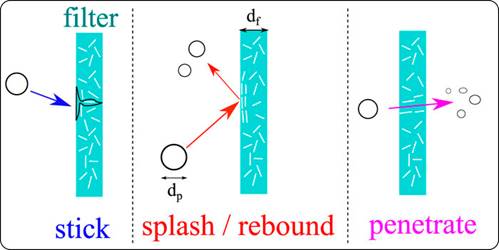
The study shows that the criteria employed for
assessing the face mask performance must be
modified to take into account the penetration
dynamics of airborne droplet transmission, the
fluid dynamics leakage around the filter, and
reduction of efficiency during cough cycles. A
new criterion for calculating more accurately
the mask efficiency by taking into account the
penetration dynamics is proposed. We show that
the use of masks will reduce the airborne
droplet transmission and will also protect the
wearer from the droplets expelled from other
subjects.
However, many droplets still spread around and
away from the cover, cumulatively, during cough
cycles. Therefore, the use of a mask does not
provide complete protection, and social
distancing remains important during a pandemic.
The implications of the reduced mask efficiency
and respiratory droplet transmission away from
the mask are even more critical for healthcare
workers. The results of this study provide
evidence of droplet transmission prevention by
face masks, which can guide their use and
further improvement.
https://aip.scitation.org/doi/full/10.1063/5.0015044
Study in Israel Concludes that Masks are Used
Improperly
A recent study focusing on the habits of
personal face mask use in Israel found that
"most of the public exposes itself to infection
with COVID-19 due to wrong use of face masks."
Health experts recommend changing a mask once
every two hours. When a mask is used for too
long it can be the perfect environment for
bacterial growth, especially if after use the
mask is put on a table – another
great surface for bacteria. Doing so sets up a
never ending cycle, perfect for bacteria to
thrive in.
The survey found that 90% of the population does
not follow the creed of changing their masks
every two hours. More than 25% reported changing
their mask less than once a day, meaning a good
portion of Israelis use the same mask for days
at a time, and fewer than 10% of disposable-mask
users report using three or more masks daily.
Some 20% report changing their mask once a day.
Continuing on disposable masks, over 75% of the
population are using surgical masks while the
remainder use reusable washable masks.
As it can be seen around the world, not just in
Israel, many wearers tend to place the masks on
their neck or below their nose when not in
"use," whether by force of habit or just
flouting regulations. The survey authors note
that the neck is a place where germs and viruses
tend to accumulate throughout the day in the
life of a normal person.
The McIlvaine observation is that if 75% of the
population is wearing surgical masks that is
considerably more protection than the
cloth masks worn by most Americans.
On the other hand even surgical masks are
poor protection because of leakage. Wearing an
N95 mask for longer periods would be much safer.
The newest evidence places less transmission
from surfaces than from the air.
Respirator with HEPA Filter for Both Inhalation
and Exhalation
A
Utah company has garnered a lot of attention
online for their “microclimate” face masks,
which provide protection from the coronavirus by
surrounding a person’s head inside a filtered
bubble.
“It’s been fun to see people’s reactions,” said
inventor Michael Hall. “I will say, you have to
be comfortable in your own skin.”
Hall has been out testing the mask… a lot. His
son even wore one to school.
“I think a few people were asking you know,
‘When’s he going to Mars,’ and things like
that,” he said.
HEPA filters in the helmet clean the air coming
in and going out. Hall came up with the idea
while skiing with his family.
“We have the goggles and so I couldn’t see
them,” he said. “It really was about that
expression, of wanting to be able to look people
in the eye and talk to them.”

When the pandemic hit earlier in the year,
Hall’s team found another purpose. They’ve run
tests, showing how particulate matter gets
through cloth masks, then N95s, and finally,
through the microclimate’s filters.
Even better, Hall said you don’t have to feel
your warm breath on your face.
“I see people who have got to wear a mask all
day, and they’re usually the ones looking at it
saying, ‘how do I get that?'” said Hall.
Hall said the bubble mask is relatively
comfortable to wear.
“Kind of like eyeglasses or hats or other
wearables,” he said. “Once you have this on for
a few minutes, it just kind of disappears into
the background.”
Still, when you wear a space-helmet with those
fans running, it can have some drawbacks.
“Oh, it’s booming,” said Hall.
Hall said they’ve already had sales in the
thousands, with very little marketing.
Slate Magazine
Says Airline Case Studies are not a Worry If
People Wear Masks.
Air travel has long provoked anxiety in
passengers, but even more so after SARS-CoV-2
has taken hold worldwide. In the past several
months, scientists and public health experts
have emphasized that the risk of contracting the
virus is greatest in small, enclosed spaces with
many people—and where do people feel more
claustrophobic and crammed than an airplane?
So recently, two new case studies of potential
coronavirus transmission aboard airplanes
immediately made the rounds online, creating
buzz about the “dangers” of in-flight COVID
transmission. Several
outlets uncritically reported the authors’
findings, both published in the U.S. Centers for
Disease Control’s journal Emerging Infectious
Diseases, which looked at two clusters of
suspected coronavirus transmission on flights.
While the possibility of plane transmission may
sound alarming, neither of these studies tell us
much about COVID-19 risks that we didn’t already
know.
The first thing to note is that both cases took
place on long flights in early March. One
case study,
led by researchers at Vietnam’s National
Institute of Hygiene and Epidemiology, found a
cluster of cases on a 10-hour flight from London
to Hanoi, which landed March 2. A 27-year-old
woman had a fever and was coughing during the
flight, and the researchers later found 15 other
people on the flight who tested positive for
COVID-19. The
other study,
led by researchers in London and Hong Kong,
found that on a 15-hour March 9 flight from
Boston to Hong Kong, a couple sitting in
business class infected two flight attendants.
The length and timing of these flights
introduced potential risks that may not apply to
current air travelers. Scientists have long
emphasized exposure time as a risk factor; the
longer you’re in close proximity to an infected
person, the more likely you are to encounter the
virus particles they’re shedding. But unlike the
passengers in these clusters, most air travelers
are not taking 10- to 15-hour flights.
And the timing of these flights —early
March—means that they occurred before
mask-wearing on planes was compulsory. That’s no
longer the case; all major airlines now require
passengers to mask up. (A colleague who flew
recently told me that on her flight last week,
the pilot did not mince words about
“blacklisting” any uncooperative passengers.)
“Wearing masks makes a huge difference,” says
Qingyan Chen, professor of mechanical
engineering at Purdue University and a former
director of the FAA’s Airliner Cabin Environment
Research Center. Lab
studies have
shown that masks of all materials can be
effective at filtering virus particles and
decrease the number of particles people expel
into the air—all important factors to consider
when breathing and talking in close proximity to
other plane passengers. Hopefully, the adoption
of mask-wearing has prevented more of these
clusters from popping up.
While it’s likely these two case studies
identified cases in which COVID-19 was
transmitted aboard planes, the exact mechanisms
of transmissions are not crystal clear. In the
Boston-to-Hong Kong case, researchers performed
genetic analyses of samples from all four
infected people and found a 100 percent match,
suggesting that the couple in business class
passed on the same strain to their flight
attendants. The genome sequencing is convincing,
says Lin Chen, director of the
Harvard-affiliated Mount Auburn Hospital and
president of the International Society of Travel
Medicine. But even so, there’s still the
possibility that the crew could’ve happened to
be exposed to the same strain somewhere besides
the flight. With the London-to-Hanoi study, Chen
says she also suspects plane transmission was
likely, but the causality is even harder to
discern, because the researchers did not
sequence samples. “Until genome sequencing is
done on a lot of these suspected in-flight
transmission cases, it’s hard to say for sure.”
Joseph Allen, a researcher at the Harvard T.H.
Chan School of Public Health, laid out his
doubts about the case study’s causality in a Twitter
thread.
He points out that based on the timing of some
passengers’ symptom onset and what they did
immediately after the flight (a few went on
cruises!), it’s possible—or even likely—that
some of these “flight-associated” cases actually
contracted the coronavirus elsewhere, not
necessarily on the flight itself.
That’s not to downplay the risks of getting
COVID-19 on a plane; it can certainly happen.
But the airplane itself is not particularly
dangerous, says Purdue’s Chen. In most large
airplanes, air circulates through the cabin in
five to seven minutes, and then is filtered
through a HEPA filter that is 99.97 percent
effective at filtering small particles. “The air
supply into the cabin is super clean, but that
doesn’t mean you have zero risks there,” he
says. The biggest risk, as he sees it, is in the
moments when passengers might take masks
off—like while eating. Chen recommends
staggering snack times so that passengers don’t
all have their masks off at the same time. “The
risk occurs during this period because I talk, I
generate droplets, and that goes directly to the
people sitting next to me,” he says.
Harvard’s Chen says these studies are helpful
confirmation that flight transmission can happen,
but agrees that overall, the risk is generally
low. First, she points to the number of infected
people on these planes: Both carried more than
200 passengers, and the number of potentially
infected passengers made up just a small portion
of people aboard. And, she says, the fact that
few clusters have been reported should be
heartening, as well as the reports of cases in
which infected people have boarded an airplane
without infecting anyone.
https://slate.com/technology/2020/09/airplanes-covid-coronavirus-transmission-flying.html
BTL N95 Masks Meet All Required Test Protocols
BTL revamped several of their manufacturing
facilities to start producing
medical-grade respirators. As of
September 2020, BTL’s European manufacturing
facilities have been producing FFP2 (European
equivalent to N-95) flat-fit respirator masks,
for both medical professionals and consumers.
The respirator masks received both CE marking
and FDA EU.

The FLAT-FIT medical respirator is specially
designed to provide maximum safety without
compromising comfort. The filtration efficiency
of an FFP2 respirator is achieved by
electrostatically charged microfibers that
attract and trap airborne particles. The optimum
density of the filter membrane provides reliable
protection and low breathing resistance.
MAIN CHARACTERISTICS
|
• High filtration efficiency |
|
• Approved for use as an FFP2 respirator |
|
• Approved for use against SARS-CoV-2 according to PPE-R / 02.075 version 1 |
|
• Bacterial and Viral filtration efficiency ≥ 99.9% |
|
• Average NaCl Filtration Efficiency > 99% according to 42 CFR part 84 |
|
• Tested for splash resistance according to EN 14683 |
TECHNICAL SPECIFICATIONS
|
MODEL |
FLAT-FIT Healthcare Respirator |
|
Filter category |
FFP2 |
|
EN 14683:2019 + AC:2019 |
Splash resistance tested |
|
EN 14683:2019 + AC:2019 |
Bacterial and Viral filtration efficiency ≥ 99.9% |
|
42 CFR part 84 |
Average NaCl Filtration Efficiency > 99% |
|
PPE-R/02.075 1 version |
Approved for protection against SARS-CoV-2 |
|
Valve |
No |
Surgical Mask Leakage is a Major Hurdle to
Besting COVID
We will be placing special emphasis on assessing
the importance of leaks around the edges of
surgical masks. We will also be weighing the
alternatives from different mask designs to just
modifications and additional components.
All the latest evidence shows that much of the
COVID transmission is through small aerosols.
This means that that any leakage of air around
the mask will be dangerous. think of perfume or
cigarette smoke.
In terms of the mask preventing the escape of
virus
the problem is compounded by the
temporary capture of large droplets on the mask
interior. These droplets evaporate and will
create aerosols which will penetrate or escape
around the mask periphery. So transmission can
take place by four different routes.
Some of the answers to surgical mask leakage are
found in the Daily Alerts
Search the Daily
Coronavirus Alerts
Search
All Alerts by Headlines
Search
All Alerts by Keyword
Enter one or more keywords to search for using
the Zoom Search Engine.
Note that '*' and '?' wildcards are supported.
Search results for: surgical
81 results found.
In our August 4 Alert we reviewed mask types.
There is a technical difference between a “mask”
and a “respirator”. In day to day language we
often say mask, when referring to what are
technically called respirators.
Uses for Masks:
§ Masks are loose fitting, covering the nose
and mouth
§ Designed for one
way protection, to capture bodily
fluid leaving the wearer
§ Example – worn during surgery to prevent
coughing, sneezing, etc. on the vulnerable
patient
§ Contrary to belief, masks are NOT designed to
protect the wearer
§ The vast majority of masks do
not have a safety rating assigned to
them (e.g. NIOSH or EN)
Uses for Respirators:
§ Respirators are tight fitting masks, designed
to create a facial seal
§ Non-valved respirators
provide good two
way protection, by filtering both
inflow and outflow of air
§ These are designed to protect the wearer
(when worn properly), up to the safety rating of
the mask
§ Available as disposable, half face or full
face
§ The most
commonly discussed respirator type is
N95. This is an American standard managed by NIOSH –
part of the Center for Disease Control (CDC).
§ Europe uses two different standards. The
“filtering face piece” score (FFP) comes from EN
standard 149:2001. Then EN 143 standard covers
P1/P2/P3 ratings. Both standards are maintained
by CEN (European
Committee for Standardization).
Let’s see how all the different standards
compare:
|
Respirator Standard |
Filter Capacity (removes x% of all particles that are 0.3 microns in diameter or larger) |
|
FFP1 & P1 |
At least 80% |
|
FFP2 & P2 |
At least 94% |
|
N95 |
At least 95% |
|
N99 & FFP3 |
At least 99% |
|
P3 |
At least 99.95% |
|
N100 |
At least 99.97% |
In
our July 28 article we covered an article on
Chinese masks which showed that even if the
efficiency rating was high, the leakage during
normal activity could be 66%. Researchers first
tested each mask’s filtration efficiency by
drawing airborne diesel exhaust through a
section of the material for 30 minutes and
measuring the particulate matter and black
carbon concentrations on both sides. They also
tested four masks on 10 volunteers who were
exposed to diesel exhaust in a lab while
performing tasks such as talking, sitting,
standing, bending over and walking in place.
In
the filtration tests, the average particle and
carbon penetration ranged from 0.26 percent to
29 percent, depending on the mask material. In
the volunteers, the average leakage around mask
edges ranged from 3 percent to 68 percent during
sedentary tasks and 7 percent to 66 percent in
active tasks. Only one mask had an average
leakage below 10 percent in both active and
sedentary tests.
In
our August 4 Alert it was shown that surgical
masks were only slightly less efficient than
N95 but the study did not take into
account leakage.
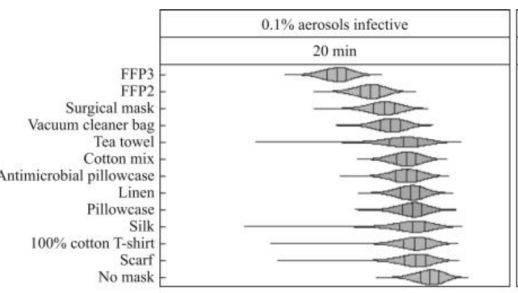
Comparing no protection (baseline) for 20-min
and 30-s exposures, it was predicted that the
mean risk of infection was reduced by 24–94% and
44–99% depending on the mask. Risk reductions
decreased as exposure durations increased. The
greatest reduction in estimated mean risk of
infection was for FFP3 masks, which reduced
baseline mean risks by 94% and 99% for 20-min
and 30-s exposures, respectively (Figure 1).
Of non-traditional materials, the vacuum cleaner
bag resulted in the greatest reduction in mean
risk of infection (20-min exposure 58%, 30-s
exposure 83%), while scarves offered the lowest
reduction (20-min exposure 24%, 30-s exposure
44%) (Figure 1).
However, large variability in filtration,
There is a direct correlation between mask
efficiency and infection risk This leads to the
conclusion that mask choice can be as important
as social distancing and other safety
measures. People should be advised not to just
wear a mask but to wear the most efficient mask
available.
In our September 14 Alert we report on use of
masks due to wildfires on the west coast. N95
masks were effective but surgical masks allowed
particles to be inhaled through openings
around the periphery.
