
Coronavirus Technology Solutions
September 30, 2020
IQ Air NanoMx and HyperHEPA Pleat Filters
Media Starting to Understand that only Efficient
Masks are Effective
Heating and Humidity to Decontaminate Masks
New York
Closes School Due to Two Cases of the
Virus
Italy Reduces Case Load with Testing of
Youngsters
Evidence Continues to Show that We Need
Efficient Masks
______________________________________________________________________________
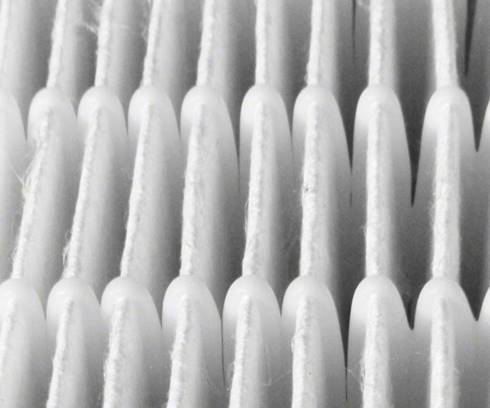
IQ Air NanoMx and HyperHEPA Pleat Filters
NanoMax filters reduce fine and ultrafine
particles by up to 95%, including viruses,
bacteria, allergens, and harmful traffic
pollutants. NanoMax filters eliminate the need
for costly upgrades to a building’s HVAC system
typically associated with HEPA filters. NanoMax
filters require no prefilters, fit into standard
2” filter slots, and have pressure drops fully
compatible with standard HVAC systems.

NanoMax filters exceed MERV 16 requirements per
ASHRAE 52.2 standards, designed to capture up to
95% of even the smallest and deadliest airborne
particles: PM2.5 (< 2.5 microns) and ultrafine
particles (< 0.1 microns), which can get into
your bloodstream and cause systemic health
effects, including dust, mold, viruses,
bacteria, allergens, and harmful traffic
pollutants.
Advanced HyperHEPA pleat design allowed IQAir
designers to build in 60 square feet of surface
area – five times more than the surface area of
a conventional pleated air filter. The result is
increased airflow and better filter loading,
which widens replacement intervals and reduces
costs.
Media Starting to Understand that only Efficient
Masks are Effective
Here are excerpts from a recent article showing
that only efficient masks are effective against
COVID.
New York, New Jersey, Maryland, and other states
are requiring everyone to wear a mask or a
substitute face covering to leave home. The
federal Centers for Disease Control and
Prevention has suddenly flipped from urging the
public not to wear masks to recommending that
they wear something that covers their nose and
mouth.
New York's Mayor Bill de Blasio's new signature
look is a western-style bandana pulled up over
his mouth and nose. No doubt he's
well-intentioned. But that kind of face-covering
is only a hair better than no covering at all.
Science shows it's a mere 2% to 3% effective.
It's misleading.
From Day One of the coronavirus outbreak, the
public has gotten the run around about masks.
Government officials need to be honest about
what works and what doesn't. Here's the
scientific evidence:
N95 masks, which are molded and fit tight to the
face, filter out 95% of viral particles, even
the smallest ones. These masks offer the best
protection, but they are in short supply, and
public officials want them reserved for health
care workers on the front lines.
Surgical masks, the kind you see commonly worn
in hospitals and dentists' offices, are flat and
held to the face with elastic. They're made from
a nonwoven material, polypropylene, that is a
somewhat effective filter. They protect the
wearer from about 56% of viral droplets emitted
by an infected person nearby, according to
research in the British Medical Journal.
Not so woven cloth masks. They allow in 97% of
viral particles. That means almost no protection
for the wearer.
Wearing a homemade cotton mask is a false
assurance, explains epidemiologist May Chu. She
says it will block only about 2% of airflow.
Similarly, a study in Disaster Medical and
Public Health Preparedness concludes that a
homemade mask should be considered "only as a
last resort," better than no protection at all
but not a lot better.
Surgical masks seem available in stores now, and
if you can buy a supply, using them is far
preferable to make your own. Don't reuse the
mask and avoid touching the outside of the mask,
because it's likely contaminated after use.
If you have to resort to homemade barriers, keep
in mind that the more layers of cloth, the
better the protection. Four layers likely block
out 13% of viral droplets, compared with the 2%
blocked with a single layer, according to a
study in Aerosol and Air Quality Research.
Why are public officials suddenly urging mask
use, many weeks after the coronavirus struck?
Because of mounting research pointing to the
huge role of asymptomatic people spreading the
disease before they feel ill. Whenever these
asymptomatic carriers talk or simply exhale,
they spread very small droplets of virus-laden
saliva and respiratory mucous in the air.
Scientists call it bioaerosols.
Getting everyone to mask up does double duty --
helping to protect the uninfected and keeping
the unknowingly infected from spreading the
virus. As New York Governor Andrew Cuomo said,
announcing the mask mandate: "You don't have a
right to infect me."
That makes sense, but Americans have had to put
up with a lot of message confusion from the
outset, and now they're getting misleading
advice about homemade masks.
What's the root problem? Year after year after
year, through three presidencies, federal health
bureaucrats ignored warnings about inadequate
supplies of masks and other equipment in the
event of a pandemic. Ten federal reports sounded
the alarm, even as the nation witnessed SARS,
MERS, avian flu and swine flu that circled the
globe. In 2009, during the swine flu outbreak,
the federal Strategic National Stockpile
dispersed 85 million N95 masks, as well as other
protective masks. The masks were never replaced.
Don't blame any president, Democratic or
Republican, for this oversight. The career
officials at Health and Human Services knowingly
allowed the nation to be undersupplied. They
never requested enough money to adequately stock
the Strategic National Stockpile. Their agenda
was global, tracking down polio in Pakistan,
pouring nearly $5 billion in the fight against
Ebola overseas and funding a Global Health
Security Agenda serving 49 countries. But no
masks for Americans.
When the coronavirus struck, the CDC offered
only mask double talk. The agency said, on the
one hand, masks are vital to protect health care
workers, and on the other hand, masks won't make
the public safer. It defies common sense. The
agency should have leveled with people,
admitting supplies had to be saved for front
line caregivers.
The coronavirus could return next winter. Or
another viral pandemic could strike from any
part of the globe. The bill Congress enacted in
late March allocates $16 billion to the
Strategic National Stockpile, nearly 30 times
its annual budget. Next time, the U.S. will have
enough masks.
Heating and Humidity to Decontaminate Masks
Scientists out of Department of Energy’s SLAC
National Accelerator Laboratory, Stanford
University and the University of Texas Medical
Branch have now found a technique, which could
allow the masks to get disinfected and make it
safer for reuse.
According to researchers, something simple as
'heating' the mask could relatively disinfect
the virus and help recycle them for further use.
The strategy, which researchers feel which
definitely help healthcare workers at a time
like this could lessen the shortage problem and
not contribute to the pandemic pollution as
well.
“You
can imagine each doctor or nurse having their
own personal collection of up to a dozen masks.
The ability to decontaminate these for reuse
would ease the shortage.
While there are no studies yet to confirm the
reaction of the novel coronavirus in contact
with high temperatures, scientists based out of
Stanford University devised a novel way of
combining heat and humidity to decontaminate and
inactivate the viruses at large.
Conducting the experiment in a safe environment,
scientists mimicked real-life situations by
mixing up SARS-COV-2 strains in liquids like the
fluids which come out of our mouth while a
person coughs, sneezes or breathes.
The droplet solution was then made to air dry on
a special meltblown polypropylene fibres fabric,
which is also used in the making of N95 masks
and then heated at different temperature
settings, for 30 minutes.
It was observed that the environment with high
humidity and heat was able to reduce the virus
load on the fabric. However, extreme heat
reduced the mask's sensitivity to filter out
germs and viruses.
The best temperature, for 'cooking' and rooting
out the viruses turned out to be 85-degree
Celsius, with 100% relative humidity. Scientists
were able to observe zero trace of the COVID
causing virus after sample masks were treated
under the given environment.
Additionally, it was also observed that the
method would decontaminate the mask and make it
suitable for use up to 20 times, which could
potentially help save resources.
Further, the virus killing technology could also
be useful to on other types of PPE.
New York Closes School Due to Two Cases of the
Virus
A city school has been closed for two weeks due
to the coronavirus – the first extended
shuttering this year, officials revealed
Thursday.
The John F. Kennedy Jr. school in Elmhurst is
the first city school to trigger a 14-day
quarantine protocol after it confirmed two
unrelated coronavirus cases among staffers.
Prior to the start of the academic year, the
Department of Education said it would take the
action when two or more COVID-19 infections
arise at the same school with no links between
infected students or staffers.
Administrators at the special needs high school
sent out a letter alerting parents and students
of the closure this week.
“We hope to return to the building on Wednesday,
October 13,” the message read.
Administrators said anyone who eventually tests
positive won’t return until they are no longer
infectious and that close contacts will be
instructed to quarantine.
The closure will impact 262 kids at the school
who are enrolled in a blended learning model.
All students will now learn remotely until the
doors reopen.
Mayor Bill de Blasio stressed Thursday that the
John F. Kennedy Jr. is the only one of the
city’s 1,600 schools to require a two-week
closure thus far.
The two cases were identified by City Hall’s new
“Situation Room” that monitors school
infections.
“That’s the only one the entire time that has
experienced that,” de Blasio said during his
daily press briefing. “And what’s going to
happen, I think, in a case like this is what
we’ve been telling people along those two weeks,
kids, of course, will get instruction remotely,
then the school will be a backup to everyone who
was quarantine will come right back,”
According to the DOE, 160 schools have reported
isolated coronavirus cases. In those scenarios,
schools are only required to close for 24 hours
before being allowed to reopen.
“We won’t hesitate to take quick action for the
health and safety of our school communities, and
that’s exactly what we did when two positive
cases amongst staff members were identified at
John F. Kennedy High School,” said DOE spokesman
Nathaniel Styer.
The department said that an investigation at the
school confirmed two cases among staff members
within a 7 day period.
Italy Reduces Case Load with Testing of
Youngsters
Through the window of the car in front, there's
a short, sharp cry from the toddler - eased with
a quick lollipop or a colorful picture: a
distraction aid once the swab is finished. And
then the next in a long line of vehicles pulls
up as Rome's "Baby drive-in" continues apace.
The test serves children from
newborn to the age of six. A result comes within
30 minutes. If it's negative, they can return to
day-care or school, even if there's a positive
case in their class.
It's the latest innovative initiative by the
country that was the first in Europe to be
overwhelmed by coronavirus but which is for now
managing to keep the virus in check more
successfully than many others.
Italy's cumulative number of Covid cases over
the past two weeks is currently just over 37 per
100,000 people, among the lowest rates in
Europe. The UK is at over 100, France exceeds
230 and Spain has around 330.
"February and March were very hard," says
Elisabetta Cortis, one of the pediatricians who
founded the drive-through project. "And then we
suffered a lot because with the lockdown, we had
many problems for the kids. They stayed alone -
no friends, no school, no sport, nothing."
It is actually difficult to pinpoint exactly why
Italy is somewhat bucking the trend of European
countries experiencing an alarming spike in
cases.
Its testing rate is not exceptionally high - the
UK is carrying out over three times the tests of
Italy - but the swabs are widely available and
rapid testing is now in place at some airports,
train stations and schools, so there is no sign
of the problems in accessing tests that have
been seen in the UK and elsewhere.
The most likely explanation is a combination of
factors: efficient test and tracing, a longer
lockdown - Italy was the world's first country
to shut down nationwide and among the slowest to
reopen - and the fact that the trauma of the
early weeks of the pandemic frightened Italians
into widespread compliance with rules.
At Tonarello, a pasta restaurant in the Roman
district of Trastevere, several measures are in
place, including plexiglass screens between
tables, the recording of customers' details for
contact tracing and disposable paper menus. Some
other restaurants and cafes use digital QR codes
for menu access on smart phones.
Italy was one of the slowest
countries to reopen schools - and that only now
is the hot summer beginning to break, the cold
weather bringing with it the increased risk of
contagion.
So it is possible that Italy,
ahead of the rest of Europe when Covid arrived,
is behind the curve as its neighbors struggle
with a spike.
But for now the figures look
promising. And that simple formula - tests,
rules, compliance - will, this country hopes,
halt a second wave and ease the legacy of pain
from the first.
Evidence Continues to Show that We Need
Efficient Masks
There is a battle over the importance of mask
efficiency which was reported this week in
Scientific American. In one corner, we have
scientists, epidemiologists, infectious-disease
physicians, clinicians, engineers—many different
experts in the medical community, that
is—arguing that the spread of COVID-19
by aerosols (that is, tiny droplets that can
remain airborne long enough to travel
significantly farther than the six-foot
separation we’ve been told to observe) is both
real and dangerous. In the other, it’s
the Centers for Disease Control (CDC) and
the World Health Organization (WHO), which until
very recently
have allowed only that aerosol spread is possible,
not necessarily likely.
Droplets are relatively large. Aerosols, on the
other hand, are tiny by comparison,
nearly 10,000 times smaller than a human hair.
They’re spread at far greater distances—20 to 30
feet—and can linger in the air for minutes
to hours, infecting others. What constitutes a
safe distance from aerosols is much harder to
define, especially in crowded indoor spaces with
poor ventilation. Choosing a safe mask becomes
difficult as well: an N95 respirator, for
example, would be preferable to an ill-fitting
cloth mask when it comes to filtering out these
minuscule viral aerosols. For these and other
reasons, some in the medical community suspect,
our health agencies have been reluctant to
accept the data on the airborne transmission of
COVID-19—because if they do, they’re
acknowledging a problem far more challenging
even than what we’ve been dealt with so far.
This reluctance has prompted an epic response.
In a nearly unprecedented move, 239 scientists
from 32 countries wrote an open letter to the
WHO in July, urging the agency to recognize that
airborne transmission of coronavirus by smaller
aerosol particles is possible. The
organization’s response was to subsequently
update its position, stating that aerosol
transmission “cannot be ruled out.” A glowing
endorsement this was not. The CDC,
meanwhile, posted on its Web site over the
weekend that aerosolization may be “the main way
the virus spreads,” then backtracked and removed
the content from its site, claiming the language
had been a draft of some proposed changes which
were “posted in error.”
This is a major point, not a minor one. Aerosol
carry of the virus means that any indoor area
where people gather in numbers—think
restaurants, bars, churches, schools, rallies—is
potentially a spreader of the disease, and
depending upon the numbers, a superspreader.
These are likely places with poor ventilation,
where people not only are close together but may
be speaking loudly, shouting, singing, cheering
or booing, etc.
The idea of aerosol spread is neither new nor
controversial. Several diseases,
including measles, chickenpox and
tuberculosis, have been shown to be transmitted
by aerosols. Patients sick with the flu have the
virus in their exhaled breath, and
that virus has been shown to be present in
the air. This is true for some other viruses,
including those found in infants.
Scientists in Wuhan, China, have identified
coronavirus RNA particles in the air in hospital
areas, although they haven’t yet proven that the
particles are infectious. Lab workers at the
University of Nebraska have published their
finding that they, too, have identified
coronavirus RNA in the air.
“We have pretty strong circumstantial
evidence, in a number of these superspreading indoor
incidents, that there must have been a
significant component of aerosol or airborne
transmission,” says William Bahnfleth, chair of
the American Society of Heating, Refrigerating
and Air Conditioning Engineers (ASHRAE) Epidemic
Task Force. Bahnfleth noted several examples,
including a restaurant in Guangzhou, China,
where multiple people without direct contact
with one another became infected from a single
individual, and a choir practice in Washington
state where presumed droplet and aerosol spread
from singing sickened
53 people, two of whom died.
In an e-mail interview, researcher Bjorn Birnir
shared his work, published in a preprint (a
non–peer reviewed paper), that demonstrated how
an infected person continues to exhale a cloud
of droplets and aerosols. These “build up over
time to dangerous concentrations for everyone in
the room,” Birnir says. While we don’t know
exactly how much virus is needed to infect
people or at what concentrations, these examples
show that at some point the threshold is met and
inhaled aerosols are the likely culprits.
“Aerosol transmission plays a significant role
in indoor environments and cannot be neglected,”
says environmental science expert Maosheng Yao,
a professor of engineering at Peking University.
“Sooner or later, [the WHO] is going to
recognize this officially.”
Much of the solution to the challenge of aerosol
(and droplet) transmission in indoor areas is
ventilation. “If people use recirculated air
during a pandemic, it is going to be dangerous,
because you will just circulate the virus
around,” Yao says. The goal of ventilation,
instead, is to exhaust air from inside a
building—along with whatever contaminants it
contains—and replace it with clean air from the
outside.
High efficiency air filtration and disinfection
are important. Filters should be upgraded to the
extent possible in HVAC systems without
diminishing airflow. The ASHRAE paper recommends
MERV-13 filters or the highest level allowable,
which filter very small infectious particles.
And if HVAC units cannot use higher-grade
filters, consider using portable air cleaners
with HEPA (high-efficiency particulate air)
filters to disinfect the air further.
A word about ultraviolet light. “A coronavirus
is a coronavirus,” says Bahnfleth, and
prior studies found that ultraviolet light
inactivated other coronaviruses, like SARS-CoV-1
and MERS (Middle East Respiratory Syndrome). UV
fixtures can be mounted on the ceiling or walls
or placed inside ventilation ducts to neutralize
viruses and bacteria. The biggest limitation is
that the irradiation can be a health hazard, to
both skin and eye, which is why the fixtures are
placed up high, away from people.
https://www.scientificamerican.com/article/protecting-against-covids-aerosol-threat/
