
Coronavirus Technology Solutions
August 24, 2020
More on the Photodynamic Airborne Cleaner
Working Group on Importance of Aerosol Generation on Mask and Filter Media
The Cycle from Virus Droplet Formation to Aerosol Generation in a Mask or Filter
Toilet Plume Aerosols Produced in Substantial Quantities
Urinals as Well as Toilets can be Virus Transmitters
Predicting Virus Airborne from Urinals Compared to Mask and Filter Surfaces
Virus in Air and Patient Rooms Documented in Nebraska Study
Bottom In Top Out Air Distribution Recommended for Hospital Air
______________________________________________________________________________
More on the Photodynamic Airborne Cleaner
We asked Young L Kim of Purdue to provide more details on this interesting alternative for disinfection. He told us
“Our biomedical engineering lab has developed a way to potentially neutralize viruses lingering in the air using aerosols of FDA-approved food coloring dyes. Aerosols are tiny bits of solid or liquid matter suspended in air.
Our idea was inspired by photodynamic therapy, which is a medical treatment, including for certain types of cancer. Photodynamic therapy uses a photosensitizer, a chemical that reacts with oxygen in the presence of light, to produce oxygen free radicals. These radicals are highly reactive, meaning they trigger other chemical reactions, including ones that kill harmful pathogens.
Instead of using expensive medical photosensitizers, we have identified several FDA-approved food coloring dyes that can be used to generate free radicals in visible light. We use ultrasound to generate small aerosols containing the food coloring so that the dyes can float and linger in the air. The aerosols are barely visible, and their small size and short lifespan in light means they don’t stain surfaces.
The prototype device that uses food coloring to neutralize airborne viruses being demonstrated in a classroom. Young Kim, Purdue University, CC BY-ND
We used this technique to produce a device, Photodynamic Airborne Cleaner, that disinfects pathogens floating in the air. To the best of our knowledge, this is the first-of-its-kind photodynamic therapy aerosol generator for airborne disinfection.
Viruses and bacteria are often transmitted through the air. A person infected with SARS-CoV-2, the virus that causes COVID-19, who coughs or sneezes produces virus-containing droplets and aerosols that float in the air and can cause infection.
Due to this risk, all kinds of indoor gatherings are now limited. It is critical to be able to disinfect and sanitize large volumes of indoor air where many people are present to reduce the chances of transmission.
Photodynamic therapy was first demonstrated as a means of fighting bacterial infection. Oxygen free radicals, specifically singlet oxygen, can also inactivate viruses by damaging the nucleic acids, proteins and lipids that they are composed of. In particular, singlet oxygen is effective at breaking down the lipid envelopes that form protective shells around many viruses. Most of the viruses that are harmful to humans, including SARS-CoV-2, have these envelopes.
Several other disinfection techniques are available, for example aerosolized hydrogen peroxide, hydrogen peroxide vapor, ozone, steam and UV-C or “deep UV” illumination. However, these are more appropriate for disinfecting surfaces than disabling pathogens floating in the air. Also, they can be hazardous to humans. For example, deep UV is commonly used as a disinfectant, but is carcinogenic.
We are preparing to collaborate with a federal research team to evaluate the effectiveness of our Photodynamic Airborne Cleaner against airborne transmission of SARS-CoV-2.
Aerosols of FDA-approved food coloring dyes and their singlet oxygen generation do not last for a long time. These dye aerosols break down in light, and singlet oxygen is not generated without light. Nevertheless, even though the food coloring is FDA-approved for consumption, it’s necessary to test the safety of potential inhalation and oral intake.
Working Group on Importance of Aerosol Generation on Mask and Filter Media
The question of aerosol generation from large cough and sneeze droplets on mask and filter media is of highest importance because
1. CDC guidance is to wear masks only efficient enough to capture large droplets
2. Large droplets are likely to be converted to small aerosols
3. Inefficient masks will not prevent virus spread
4. Masks and filters are needed which will prevent the newly formed aerosols from escaping
There has been no focus on this subject. Considering its importance it needs to be addressed. McIlvaine Company is therefore setting up an informal working group on Importance of Aerosol Generation on mask and filter media. For more information contact Bob McIlvaine at rmcilvaine@mcilvainecompany.com
The Cycle from Virus Droplet Formation to Aerosol Generation in a Mask or Filter
What is in large cough and sneeze droplets captured on mask and filter media? We need to analyze the whole cycle including
1. Particle inhalation
2. Droplet formation in lungs
3. Fate of captured particles in fluids
4. Particles and droplets in exhalation
5. Quantity of large droplets landing on filter media
6. Evaporation, particle impingement, air turbulence and other forces at work on droplets
7. Fate of virus originally in large droplets
The normal adult in standard room air (designated ISO 9) breathes in 7.5 million particles 0.1 microns and larger per minute. Most of these particles by count are close to the COVID in size. However these small particles do not have much weight.
Many of these particles are exhaled. Some particles are captured in fluids which are swallowed or coughed. The lungs splash droplets in their function of oxygen intake and CO2 discharge.
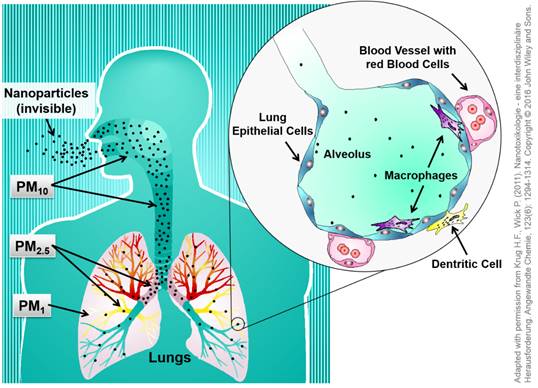
The adult human lung has a huge surface area of around 120 m2 to 140 m2 for gas exchange of oxygen and carbon dioxide. Anatomically it is made of a cascade of conducting airways, starting from the trachea, via the bronchi and bronchioli down to the gas exchange zone of the alveoli. These very small "air bubbles” are formed by epithelial cells, which are directly in contact on their interior side with endothelial cells forming the blood vessels. This alveolar barrier separates the blood within the blood vessels from the air inside the lung and can be very thin down to 200 – 500 nm.
As the breathing air contains a variety of different substances, like germs, dust particles or other contaminants, the lung has special clearance mechanisms in place to handle such contaminations. Normal air contains 1.000 up to 10.000 microbes/germs and 10 to 50 micrograms of fine and ultrafine dust particles per cubic meter. This means that an adult human who inhales 10.000 - 15.000 liter of air per day is in fact inhaling more than 10.000 microbes and more than 10 billion particles each day.
The clearance mechanisms of the body consist of two different principles, namely the alveolar macrophages and the ciliated mucociliary clearance of the upper airways. Depending on their size, particles[MM1] deposit in the different regions of the lung where they are engulfed by macrophages in the alveolar region, which move then upwards to the bronchioles and bronchi. Large particles are directly transported upwards via the mucociliary clearance, also called the mucociliary escalator. Afterwards this mucus, containing the foreign substance, is removed from the lung by coughing, swallowing or spitting.
As per the example of cigarette smoking most particles are exhaled. This would be in addition to respiratory droplets. Brownian movement of small particles will cause them to collide with droplets. If someone is wearing an N95 mask they will inhale thousands of particles per minute instead of millions. It stands to reason that less collision will take place in the exhalation.

The large droplets caught in the mask could be droplets from the lungs or mucus. Coughing will cause mucus to impinge on the mask or media surface.
There is the potential for aerosols to be transmitted either through or around the mask. The fate of the virus in these droplets will be determined by
· Droplet direct splitting
· Droplet reformation due to air flow and other forces
· Particulate collision with droplets
· Evaporation
· Penetration of salt nuclei
Droplet direct splitting: Recent work by Duke shows an example where more drops were exhaled by people with inefficient masks than people with no masks.
Droplet reformation: With 15 breaths per minute there will be turbulent air flow around the droplet
Particulate Collision: There can be a collision with larger particles being exhaled.
Evaporation will eventually reduce the droplet down to the nuclei which then may pass through the media.
This simplistic analysis is just a starting point. There are many experts such as UCSD on droplet evaporation who will be able to help put all the pieces of the puzzle together.
Toilet Plume Aerosols Produced in Substantial Quantities
The potential risks associated with “toilet plume” aerosols produced by flush toilets is a subject of continuing study. This review examines the evidence regarding toilet plume bioaerosol generation and infectious disease transmission.
The peer-reviewed scientific literature was searched to identify articles related to aerosol production during toilet flushing, as well as epidemiologic studies examining the potential role of toilets in infectious disease outbreaks.
The studies demonstrate that potentially infectious aerosols may be produced in substantial quantities during flushing. Aerosolization can continue through multiple flushes to expose subsequent toilet users. Some of the aerosols desiccate to become droplet nuclei and remain adrift in the air currents. However, no studies have yet clearly demonstrated or refuted toilet plume-related disease transmission, and the significance of the risk remains largely uncharacterized.
Research suggests that toilet plume could play a contributory role in the transmission of infectious diseases. Additional research in multiple areas is warranted to assess the risks posed by toilet plume, especially within health care facilities.
It may be concluded from the above that flush toilets produce substantial quantities of toilet plume aerosol capable of entraining microorganisms at least as large as bacteria, that sufficiently small microbe-laden droplets will evaporate to form droplet nuclei bioaerosols small enough to be inhaled deep into the lung, and that these bioaerosols may remain viable in the air for extended periods and travel with air currents. Production of these bioaerosols during multiple flushes after contamination suggests a long-term potential for a contaminated toilet to be an infectious bioaerosol generator.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4692156/
Urinals as Well as Toilets can be Virus Transmitters
This is the conclusion you reach by reading an article by Grace Hauck in USA Today. These findings are even more important when you consider that if virus is transmitted from these sources it is more easily transmitted from cough droplets on mask interiors or MERV 8 filters. In one case you have the liquid flow forces in the other you have 15 breaths per minute with some percentage of 7.5 million particles also passing both directions.
Wearing a mask in public restrooms should be mandatory during the pandemic, researchers say, because there's increasing evidence that flushing toilets – and now urinals – can release inhalable coronavirus particles into the air.
The coronavirus can be found in a person's urine or stool, and flushing urinals can generate an "alarming upward flow" of particles that "travel faster and fly farther" than particles from a toilet flush, according to a study published in the journal Physics of Fluid Monday.
"Urinal flushing indeed promotes the spread of bacteria and viruses," researcher Xiangdong Liu said in a press release. "Wearing a mask should be mandatory within public restrooms during the pandemic, and anti-diffusion improvements are urgently needed to prevent the spread of COVID-19."
Liu and other researchers from Yangzhou University in China simulated urinal flushing using computer models and estimated that, within just five seconds of flushing, virus particles could reach a height of more than 2 feet off the ground.
"Potentially, it could contaminate other surfaces you would touch – the handle, the tap," said Charles Gerba, a professor of virology at the University of Arizona. "The concern is also – was there anything left over from the person who was there before? Aerosolization from the previous user you may potentially inhale?"
Some of the same researchers released similar findings in June, focused on toilet flushing. Through another computer model, the researchers found that thousands of particles can come out of the toilet within 70 seconds of flushing, and that some can reach higher than a foot above the toilet bowl in half that time.
"It is reasonable to assume that the high-speed airflow will expel aerosol particles from the bowl to regions high in the air above the toilet, allowing viruses to spread indoors causing risks to human health," the researchers said at the time.
The studies are interesting but unsurprising, as research on particles kicked up in "toilet plumes" has been around for about two decades now, said Joshua Santarpia, a professor of pathology and microbiology at the University of Nebraska Medical Center specializing in bioaerosols.
"The more interesting thing to me was that I hadn’t considered the urine issue – whether SARS-CoV-2 was shed in urine," he said.
Many people aren't aware that toilets and urinals can release particles into the air, let alone that genetic material from SARS-CoV-2 – the virus that causes the disease known as COVID-19 – can be found in patients' urine and stool, Gerba said.
"It’s probably been overlooked – urine contamination," Gerba said. "Smallpox, Zika virus are excreted in the urine. What’s surprising is that a respiratory virus can be excreted in the urine."
At least two studies – one in Tokyo and one in Guangzhou, China – have found coronavirus RNA in patients' urine. Studies published in the journals Gastroenterology and The Lancet also found coronavirus RNA in patients' stool, even weeks after the patients showed negative results in respiratory samples. One study in and around Beijing, however, did not find any evidence of virus in 72 urine specimens.
It's still unclear whether COVID-19 can transmit through urine and infect another person, Gerba said.
"Is there enough virus in the urine to worry about? Does enough get aerosolized? Those are questions we need to look at," he said.
The researchers at Yangzhou University argue that transmission in a public restroom has already happened. They cite local news reports of a couple, who work at a food market in Beijing, contracting the virus at a restroom nearby.
"What’s worse, two of COVID-19 reemerging confirmed cases in Beijing have been reported to be infected from a public toilet, which practically proves the danger from the public restroom," the researchers wrote.
Health experts believe the virus mainly transmits through respiratory droplets when someone coughs or sneezes, but the World Health Organization says that "short-range aerosol transmission . . . cannot be ruled out."
Researchers measuring the amount of viral aerosols in different areas of two Wuhan hospitals found that while the concentration detected in isolation wards and ventilated patient rooms was very low, it was higher in the toilet areas used by the patients, according to an April study published in the journal Nature.
The researchers recommended that room ventilation, open space, sanitization of protective apparel, and proper use and disinfection of toilet areas could effectively limit the concentration of SARS-CoV-2 RNA in aerosols.
"I think there’s a lot of strategies and interventions that could be developed if it really turns out that there’s significant risk," Gerba said.
For now, the next best step would be to put the researchers' computer model to the test to see if flushing a urinal actually kicks virus particles up into the air, Gerba and Santarpia said.
"Somebody should really validate some of this experimentally. It’s a model, and there are a lot of assumptions," Santarpia said. "More work needs to be done."
Follow Grace Hauck on Twitter at @grace_hauck.
Predicting Virus Airborne from Urinals Compared to Mask and Filter Surfaces
Let’s examine the physical conditions and compare them to masks in the above article where Urinal flushing indeed promotes the spread of bacteria and viruses," according to researcher Xiangdong Liu. How do the liquid flow forces in the urinal compare to the air flow forces in a mask. It is a valid suggestion since the authors point out that the same model was used for coughs.
Similar to the flushing of the toilet, the flushing process of the urinal involves significant interactions between the gas and liquid interfaces. Therefore, this Letter adopts the VOF model to track and characterize the two-phase interface in which the realizable k–ε turbulence model is accepted. In addition, the flow pattern of virus aerosols under the urinal flushing is reflected by the DPM model, a Lagrangian scheme, which has successfully simulated the human cough-induced flow and sprayed droplet flow. Please refer to the work by Li for the detailed math formulations.
During simulation, several assumptions are adopted: (1) there are no heat and mass (evaporation) interactions between the particles and the air and liquid phases; (2) generation of the aerosol particles during the flushing is ignored; (3) physical properties and size of the aerosol particles are constant; and (4) the temperature remains to be 20 °C.
This effort should be helpful in analyzing the aerosol generation of viruses from cough droplets on masks and filters.
https://aip.scitation.org/doi/10.1063/5.0021450
Virus in Air and Patient Rooms Documented in Nebraska Study
A study by University of Nebraska Medical Center researchers provides new evidence of infectious SARS-CoV-2 throughout the environment and in air samples collected in COVID-19 patient care areas.
This wide dissemination also supports the concern about cough droplets landing on a cloth mask or MERV 8 filter. With 15 breaths per minute or continuous air flow the dispersion of the virus seems to even be more likely than some of the routes documented in this study.
The scientists, funded by a U.S. National Science Foundation rapid response grant, published their results in Nature Scientific Reports.
During the initial isolation of 13 people confirmed positive with COVID-19, air and surface samples were collected in 11 isolation rooms to examine environmental contamination.
The researchers found viral contamination on all commonly used surfaces in the rooms, and very high levels of the virus in the air grates. Air samples from hallways outside patient rooms, where staff members were moving in and out, were also positive.
Evidence of the virus in the air and on many commonly used items, including bathroom facilities, indicates that SARS-CoV-2 is widely disseminated in the environment.
The results of the research suggest that COVID-19 patients, even those who are only mildly ill, may spread the virus and contaminate surfaces that pose a risk of transmission. The results also suggest that airborne isolation precautions are appropriate.
"Studies like this are needed to understand proper precautions for healthcare workers, first responders and others who care for the ill and are needed to combat this pandemic," said Joshua Santarpia, a pathologist and microbiologist at the medical center. "This ongoing work will continue to improve our understanding of SARS-CoV-2 transmission and help identify ways to improve safety in the care of patients with COVID-19."
The researchers stress that careful environmental cleaning and disinfection of surfaces, including those in bathrooms, is important. They recommend that appropriate personal protective equipment, including respiratory protection, be used in the treatment of people known or suspected to be infected with SARS-CoV-2.
"This study increases our knowledge of the stability and spread of SARS-CoV-2 in indoor environments," says Joanna Shisler, a program director in NSF's Division of Integrative Organismal Systems. "The information can help us understand how to clean and maintain rooms and buildings to decrease possible virus transmission."
https://www.nsf.gov/discoveries/disc_summ.jsp?cntn_id=301008&org=NSF&from=news
Bottom In Top Out Air Distribution Recommended for Hospital Air
Considering the hospital is the most “dangerous” place to occur massive cross-infection among patients as emerging virus usually comes in a disguised way, an air distribution optimization of a general three-bed hospital ward in China is carried out in this paper.
Using the Eulerian-Lagrangian method, sneeze process from patients who are assumed to be the virus carrier, which is responsible for a common event to trigger cross-infection, is simulated. The trajectory of the released toxic particle and the probability of approaching others in the same ward are calculated. Two evaluation parameters, total maximum time (TMT) and overall particle concentration (OPC) to reflect the particle mobility and probability to cause cross-infection respectively, are developed to evaluate the proposed ten air distributions in this paper. A relatively optimized air distribution proposal with the lowest TMT and OPC is distinguished through a three-stage actively analysis.
Results show that a bottom-in and top-out air distribution proposal is recommended to minimize the cross-infection.

