
Coronavirus Technology Solutions
August 21, 2020
COVID Will Require Permanent Adjustments Says WHO
Saliva Test Could be a Game Changer
Testing Already Launched at U of I Urbana
Airborne Transmission Workshop, August 26 and 27
Disinfection Using UV Light and Nanoscan3 from Sick
Sweden Doesn’t Recommend Face Masks But is Paying the Price
_________________________________________________________________________
COVID Will Require Permanent Adjustments Says WHO
The World Health Organization said Friday that a vaccine will be a "vital tool" in the global fight against the coronavirus, but it won't end the Covid-19 pandemic on its own and there's no guarantee scientists will find one.
World leaders and the public must learn to manage the virus and make permanent adjustments to their daily lives to bring the virus down to low levels, WHO Director-General Tedros Adhanom Ghebreyesus said during a news conference from the agency's Geneva headquarters. "At the same time, we will not, we cannot go back to the way things were."
Throughout history, outbreaks and pandemics have changed economies and societies, he said.
"In particular, the Covid-19 pandemic has given new impetus to the need to accelerate efforts to respond to climate change," he said. "The Covid-19 pandemic has given us a glimpse of our world as it could be - cleaner skies and rivers."
The virus has infected more than 22.7 million people worldwide and killed at least 794,100 in more than seven months, according to data compiled by Johns Hopkins University. There are at least 30 potential vaccines currently in clinical trials, according to the WHO, but there is no guarantee they will be safe and effective, he said.
Even though human trials for potential vaccines are progressing, scientists say key questions remain. Covid-19 was discovered in December. While numerous research papers and studies have been produced on the virus, scientists still don't fully understand how it affects the body or how well someone is protected from reinfection after recovering.
Earlier this month, Tedros said there was no "silver bullet" to the coronavirus and "there might never be."
He said world leaders can stop new outbreaks by practicing the "basics" of public health and disease control. "Testing, isolating and treating patients and tracing and quarantining their contacts. Do it all. Inform, empower and listen to communities. Do it all," he said Aug. 3.
Tedros said Friday that "every single person" can make a difference in the pandemic.
"Every person and family has a responsibility to know the level of Covid-19 transmission locally and to understand what they can do to protect themselves and others," he said.
Dr. Maria Van Kerkhove, head of the WHO's emerging diseases and zoonosis unit, said it's "very important" for the public to learn "how to live with this virus."
That will help "continue to suppress transmission, identify cases and clusters that pop up so we can quickly put those out and minimize as many deaths as possible," she said. "In doing so, some countries may need to implement some measures again."
Van Kerkhove said some countries, using data, are now choosing to implement social distancing measures in areas where there is a high level of transmission.
"What we are seeing now is a targeted approach to adding interventions that need to be put in place to get outbreaks under control and reduce the number of infections that are happening," she said.
Saliva Test Could be a Game Changer
A saliva-based COVID-19 test developed by the University of Illinois has received emergency authorization from the U.S. Food and Drug Administration, creating the potential for widespread use of a test experts say is faster, cheaper and simpler.
“This has potentially game-changing implications for our statewide testing complex as well as for testing on a national level, particularly for our high-risk communities and settings,” Gov. J.B. Pritzker said at a news conference Wednesday where he characterized the announcement as “some of the best news that we’ve had since this pandemic began.”
Health experts also praise saliva tests for often requiring fewer testing materials — including chemical reagents, swabs and personal protective equipment — which have been in short supply amid the pandemic.
Dr. Martin Burke, an associate dean for research at the (U. of I.) Carle Illinois College of Medicine, said he was given the task in March of creating a team to “try to stand up and strategically deploy scalable COVID-19 testing.”
“The standard process is too slow. It’s too expensive, and it has too many supply chain bottlenecks in order to be able to do fast and frequent testing on scale,” Burke said.
Scientifically, there’s increasing evidence that “this is the medium that matters,” Burke said of saliva-based testing.
“We spread COVID-19 through saliva droplets, primarily, so you’re testing the exact medium in which that infectiousness is likely to occur,” Burke said. “It’s also much easier to collect, it requires less PPE, doesn’t necessarily require direct engagement with the health care worker and as we’ve shown, the process can be done very fast.”
In many cases, the results are available within three to six hours, while other tests continue to have lags of days, or more than a week in some cases, before results are available.
The FDA has previously granted approval to other saliva-based tests. The green light for the U. of I. test came after a “bridging study” that found it performs at least as well as a similar test developed by Yale University. The FDA granted emergency-use authorization for Yale’s test on Saturday, and the U. of I. test was placed under the same umbrella.
Yale researchers partnered with the National Basketball Association, whose players and staff have routinely taken the saliva test before and during isolation in the NBA bubble in Florida, as part of a COVID-19 testing study.
“Providing this type of flexibility for processing saliva samples to test for COVID-19 infection is groundbreaking in terms of efficiency and avoiding shortages of crucial test components like reagents,” said FDA Commissioner Dr. Stephen Hahn, referencing the Yale saliva test.
The Illinois-developed test is “different enough that it has unique features that make it very well-suited for scalability,” Burke said, adding that the test’s cost is about $10 apiece, “which is a substantial reduction in cost relative to currently what’s being utilized.”
The FDA granted emergency-use authorization to Rutgers University researchers in April for their saliva-based test, which was the first one to receive federal approval.
Illinois daily case numbers have approached late May levels several times in recent weeks after remaining fairly consistently below 1,000 in parts of June and early July.
Testing Already Launched at U of I Urbana
Martin Burke, (see previous article) at the University of Illinois at Urbana-Champaign has already launched a similar saliva test he developed at the university’s campus to screen more than 50,000 students, faculty and staff members. The test’s quick turnaround time has allowed the school to reach its goal of 20,000 tests per day, or its aim to test students twice per week.
Millions of students are returning to college campuses this fall, and some have already been sent home because of outbreaks. As schools have wrestled with implementing coronavirus precautions and screening, Burke believes the speed and affordability of the saliva test could be scalable for others — if they have the availability of a lab. Frequent testing would guarantee an infected person is notified and quarantined promptly before passing the virus to peers.
Illinois students can go to one of 40 testing stations across their campus, self-administer the test and get their results on a university-created app within three to five hours, Burke said. The school retrofitted its veterinarian laboratory to handle screening the student population. Burke hopes the capacity will be expanded to offer testing to other people off-campus.
While Burke’s team is still collecting data on the test’s sensitivity, he said that an initial clinical study showed promising results.
Prompt and persistent screening is essential to reducing the “window of transmission,” allowing those who are infected to isolate early before exposing others.
“If you look at the goal of surveillance testing, fast and frequent testing is the key,” Burke said.
The test is also cheaper since it doesn’t need some finite reagents. The Yale researchers estimated the test could cost up to $10 to be run.
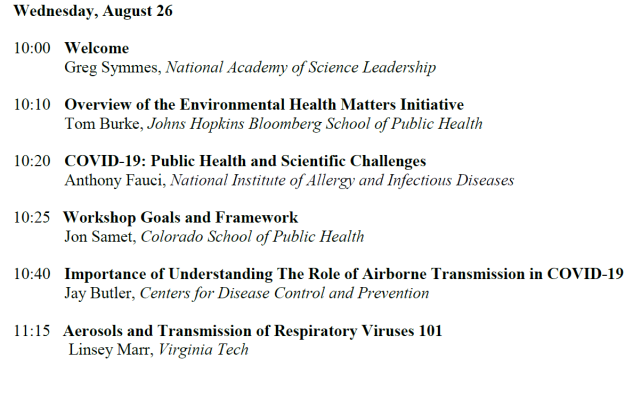
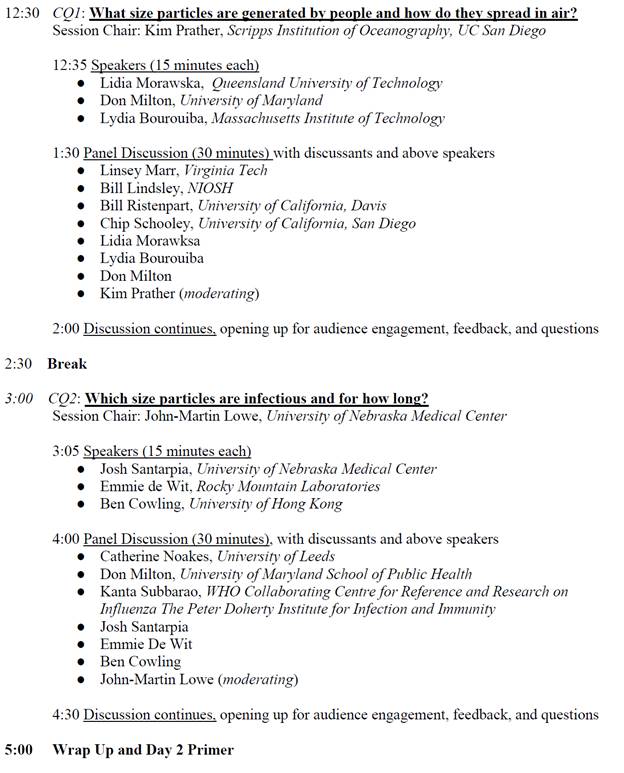
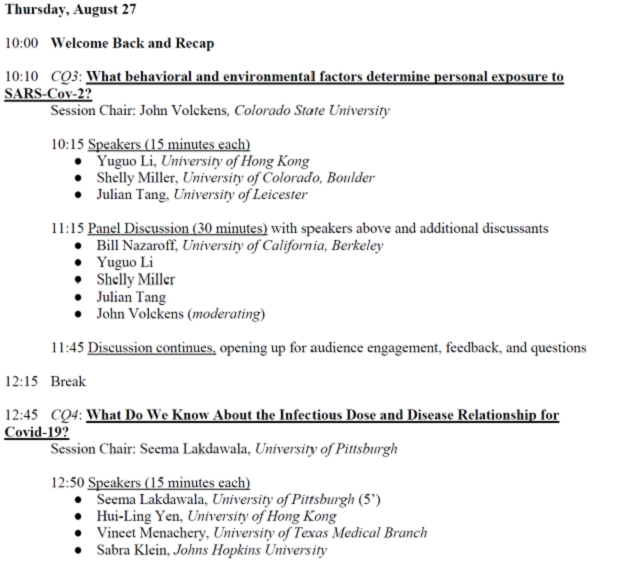
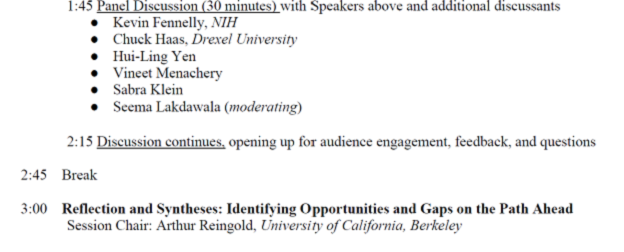
Airborne Transmission Workshop, August 26 and 27
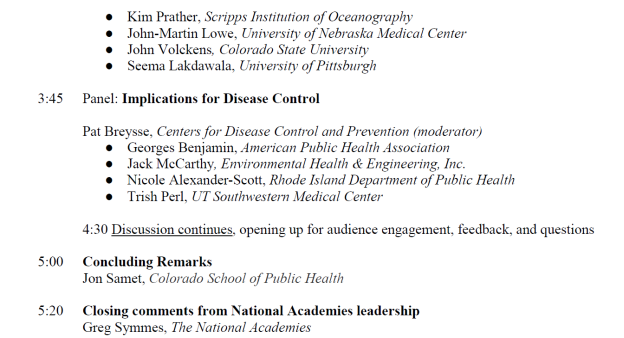
There is much we don’t know about the transmission of SARS-CoV-2, the virus that causes COVID-19. We know it can spread from an infected person’s sneeze or cough. But what do we know about transmission via speech and exhaled breath? How long do infectious particles linger in the air? How far can they travel? This Environmental Health Matters Initiative (EHMI) workshop will delve into the rapidly evolving science on the spread of the virus, as part of a larger body of COVID-19 related work at the National Academies. It will feature experts in aerosol science, virology, infectious disease, and epidemiology.
The workshop will take place over two days, both of which will last from 10:00am ET to 5:30pm ET. Visitors will only need to register through Eventbrite once to receive participation information for both days of the workshop.
Disinfection Using UV Light and Nanoscan3 from Sick
Sunglasses and sunscreen protect us from it during summer. For viruses, however, there’s no escaping it. We’re talking about UV light. As damaging as it may be for the skin and eyes, its destructive effect on viruses is very useful. That's why UV light is regularly and successfully used these days, in particular for the disinfection of rooms. And to protect humans in this application as well, some ingenious people have developed robots for the task. The Chinese start-up Youibot selected the nanoScan3 from SICK as a tried-and-proven solution for controlling mobile platforms.

While the hunt is on globally to find solutions for stopping the pandemic and possibly developing a vaccine, UV light is being employed more and more often for disinfecting surfaces and rooms. Companies all around the world are working on mobile surface disinfection solutions based on UV light. So too the Chinese start-up Youibot, which has developed a disinfection robot. The somewhat martial arts suggestive name “ARIS-K2 Virus Killing Robot” refers unmistakably to the most important function of this new development. But it also features particular “intrinsic qualities”, to which SICK as a partner has contributed in the form of the nanoScan3. These ensure, amongst other things, that the robot can carry out its work without actually posing any hazard to the people involved.

Equipped with a nanoScan3, the ARIS-K2 moves safely around the room like a mobile platform. The nanoScan3 is the smallest safety laser scanner from SICK. It is perfectly suited for the protection and localization of mobile platforms. The ease-of-use of the Safety Designer configuration software and the intelligent integration options it provides were an additional plus point for the Chinese robot builders. They provide a high degree of flexibility and save time, including during the implementation of the disinfection application. “We are very pleased to have had the opportunity to support Youibot in implementing this robot in such a short time. Using our nanoScan3, it is certain to navigate around safely on its disinfection rounds”, summarizes Benny Liu, the responsible product manager at SICK.
In addition to the UV lamps, the mobile robot is also equipped with a thermal camera. This enables it to perform two functions: during the day the robot checks the body temperature of passers-by, and during the night it uses its vertically mounted lamps to disinfect, for example, empty production halls. “Its main applications include shopping centers, manufacturing plants, and any areas where lots of people come together”, explains Benny Liu. This fascinating robot is already irradiating factories, airports, and a hospital – a true ray of hope on the horizon. And with the nanoScan3 onboard, always on the safe side while doing so.
Sweden Doesn’t Recommend Face Masks But is Paying the Price
Sweden recorded its highest death tally in 150 years for the first half of 2020, according to the country's official statistics office.
Between January and June this year, 51,405 deaths were registered -- more than 6,500 fatalities (or 15%) over the same period in 2019.
This is the highest number of deaths in Sweden during the first half of the year since 1869, when the country was struck by famine and 55,431 people died.
The country also experienced the lowest population increase since 2005, with a surplus figure of 6,860 in 2020 that was less than half that of the previous year.
Immigration figures saw a reduction of 34.7% from the same period in 2019, with the figures primarily dropping in the second quarter between April and June.
Unlike most countries, Sweden did not go into a lockdown when the pandemic spread across Europe in early spring. Instead, there was an emphasis on personal responsibility, with most bars, schools, restaurants and salons remaining open.
Despite the more relaxed approach, only 7.3% of people in Stockholm had developed the antibodies needed to fight the disease by late April -- well below the 70-90% needed for herd immunity.
By early June, the country's coronavirus death toll was at more than 4,500. According to Johns Hopkins University, it now stands at 5,802.
Much of the criticism around Sweden's response has focused on the high death rates in care homes. Sweden's chief epidemiologist Anders Tegnell admitted in June that the country's Public Health Agency "didn't know that there would be such a big potential for the disease to spread in elderly care homes, with so many deaths."
But he told Swedish newspaper Dagens Nyheter: "There are things that we could have done better but in general I think that Sweden has chosen the right way."
In an interview with CNN's Christiane Amanpour in July, Tegnell again defended the country's approach. "I think that we still believe the strategy has served us very well in many different aspects," he said.
"I know that the death toll is very high. It's not extremely high if you compare it to countries like Belgium, Netherlands, or UK, which are countries which in many ways have a much more similar epidemic than our neighboring Nordic countries.
"There is really no proof that saved people in long-term care facilities in Sweden."
He said that when the authorities saw the problems in care homes, advice was distributed and cases dropped quickly and were now almost at zero.
Tegnell on Thursday explained that Sweden was not recommending the use of face masks, which are considered key to reducing the spread of the virus by many other countries, because they could encourage people to take more risks.
"It is very dangerous to believe face masks would change the game when it comes to Covid-19," Tegnell told the Financial Times.
"Face masks can be a complement to other things when other things are safely in place. But to start with having face masks and then think you can crowd your buses or your shopping malls -- that's definitely a mistake," he added.
Sweden has also paid a heavy economic price, despite not locking down. Hospitality and tourism businesses told CNN they had taken a huge hit, and manufacturers have been cut off from international supply chains.
Nearly 50% of the country's economy is largely built on exporting goods overseas, and the global crisis has destroyed international demand.
Sweden's economy is predicted to contract by more than 5% with hundreds of thousands losing jobs.
