Coronavirus Technology Solutions
July 27, 2020
Abhishek Saha Interview on Droplet Travel
Program to Make the Best Coronavirus Decisions Should Implemented Now and Then Continuously Improved
Turning Off Air-Conditioning is Not a Good Idea
AAF Tests Efficiency of Virus Removal for Various Filters
MERV 16 Filters are a Better Choice to Mitigate COVID
______________________________________________________________________________
Abhishek Saha Interview on Droplet Travel

Summary
Abhishek Saha, Assistant Professor at University of California San Diego, explained that modeling shows respiratory droplets from a cough or sneeze travel farther and last longer in humid, cold climates than in hot, dry ones. This is the conclusion of a study on droplet physics by an international team of engineers. The researchers incorporated this understanding of the impact of environmental factors on droplet spread into a new mathematical model that can be used to predict the early spread of respiratory viruses including COVID-19, and the role of respiratory droplets in that spread.
The team developed this new model to better understand the role that droplet clouds play in the spread of respiratory viruses. Their model is the first to be based on a fundamental approach taken to study chemical reactions called collision rate theory, which looks at the interaction and collision rates of a droplet cloud exhaled by an infected person with healthy people. Their work connects population-scale human interaction with their micro-scale droplet physics results on how far and fast droplets spread, and how long they last.
A second model is being developed to determine evaporated droplet nuclei spread.
Abhishek and Bob McIlvaine then discussed how the model could be used to determine the small droplet and nuclei travel resulting from the initial capture of a large cough or sneeze droplet on the interior surface of a cloth mask. There was agreement of the likelihood that if the large droplet is initially captured in a mask with relatively large pores that small droplets may be generated by further exhalation along with evaporation. The group will be continuing their studies and would be open to funding to investigate this important phenomenon.
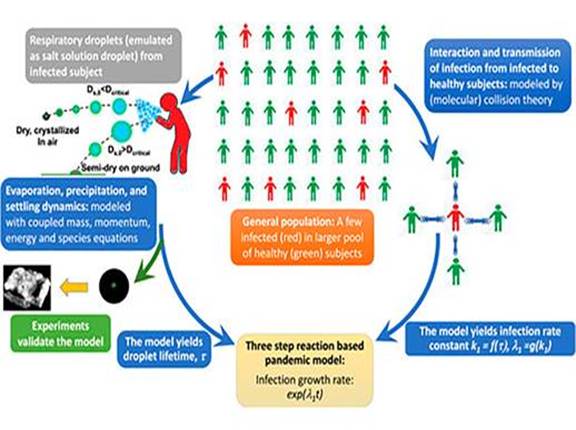
“The basic fundamental form of a chemical reaction is two molecules are colliding. How frequently they’re colliding will give you how fast the reaction progresses,” said Abhishek Saha, a professor of mechanical engineering at the University of California San Diego, and one of the authors of the paper. “It’s exactly the same here; how frequently healthy people are coming in contact with an infected droplet cloud can be a measure of how fast the disease can spread.”
They found that, depending on weather conditions, some respiratory droplets travel between 8 feet and 13 feet away from their source before evaporating, without even accounting for wind. This means that without masks, six feet of social distance may not be enough to keep one person’s exhalated particles from reaching someone else.
To view this YouTube recording click here: https://youtu.be/F790vEfB4ws
Program to Make the Best Coronavirus Decisions Should Implemented Now and Then Continuously Improved
Decisions such as opening schools and malls are being made without guidance as to the risk mitigation with various technology solution alternatives. Installing partitions without regard to air direction, turning off air conditioning or even wearing inefficient masks increases risk.
The McIlvaine Company is attempting to determine the best combination for each situation. The challenge is the large number of variables including technologies and products. There are a number of companies and institutions up to meeting this challenge. We are identifying them and reporting their insights in our Daily Alerts. But we have to put this knowledge into a framework which delivers the best recommendations at any given time.
We start with the holistic approach which assigns values to life duration and quality and economic impacts. McIlvaine has this structure. It was first created in a project for Cardinal Health relative to single use gowns and is explained at Sustainability Universal Rating System.
The next step is to make available the knowledge from air pollution control, cleanrooms and industrial hygiene. When we do that we realize for example mask and filter efficiency is much more important than has been assumed.
Here is the standard that the cleanroom industry uses to classify rooms. The cleanest reduces the number of particles less than 0.1 microns to 10. This compares to room air which has 1 billion particles per m3.
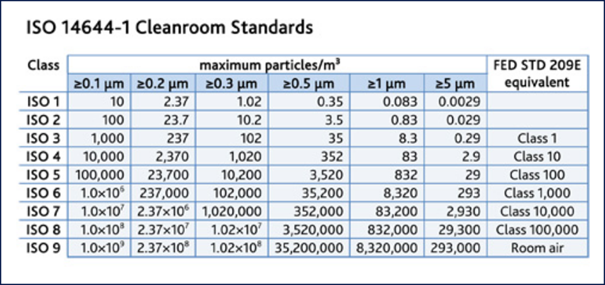
This means that if you are wearing an inefficient mask you are inhaling and exhaling billions of particles. From the air pollution control industry we know that some of these particles (e.g. mercury) may have originated in a gold mine in Brazil and ended up in the Artic. COVID has shown up on air pollution particles in the Lombardi region of Italy. Several studies show greater COVID infection rates in areas of high air pollution. But this may be due to weakened immune systems.
It may be unlikely but possible that a small particle you exhale could be inhaled by someone in China. Assumedly any virus would not be active but on the other hand some studies show that virus is at times dormant and is activated by moisture in the lungs.
The average individual in a room of average air purity will breath in and exhale many millions of particles every minute. Here are the particles by size in each breath.
|
Particles in Room Air and in Breath |
|||
|
Particle diameter greater than or equal in micrometers |
Number of particles per cubic meter |
Particles per breath -Tidal volume- 0.5 liters |
Particles per minute exhaled based on 15 breaths /min |
|
0.1 |
1,000,000,000 |
500,000 |
7,500,000 |
|
0.2 |
237,000,000 |
118,000 |
1,770,000 |
|
O.3 |
100,020,000 |
50,010 |
750,150 |
|
0.5 |
35,000,000 |
17,500 |
262,500 |
|
1 |
8,320,000 |
4160 |
62,400 |
|
5 |
293,000 |
147 |
2205 |
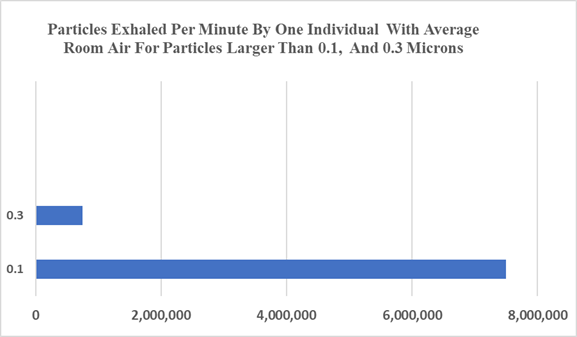
If someone is wearing a cloth mask he will be inhaling and exhaling as many as 8 million particles per minute. With an N95 mask the number would be greatly reduced
Some experts estimate that exposure to as few as 1000 SARS-CoV-2 viral particles can cause an infection. This dose of virus could occur by inhaling 1000 infectious viral particles in a single breath, 100 viral particles in 10 breaths, or 10 viral particles in 100 breaths.
A single cough releases about 3,000 respiratory droplets that travel at 50 miles per hour. Without a mask most droplets are large, and quickly fall to the ground, but many remain airborne and can travel across a room in a few seconds. With a mask the large droplets are captured on the mask interior and become aerosol generators. A single sneeze releases about 30,000 droplets traveling up to 200 miles per hour. Most droplets are small and travel great distances. The droplets from a single cough or a sneeze emitted by an infected person may contain as many as 200,000,000 virus particles. It stands to reason that most of these virus particles will be discharged from the inefficient mask in subsequent exhalations.
Breathing may release as few as 20 to 30 viral particles per minute. Speaking increases the release of respiratory droplets about tenfold more than breathing; 200 virus particles per minute. A person could become infected after ten minutes of face to face talking with an infected person. Experts are agreed that inefficient masks do not capture the small aerosols caused by breathing and speaking.
Since air can contain millions of viruses it is necessary to develop robust programs which can deal with large numbers.
The collision rate theory described in our interview with UCSD provides a holistic modeling approach https://youtu.be/F790vEfB4ws
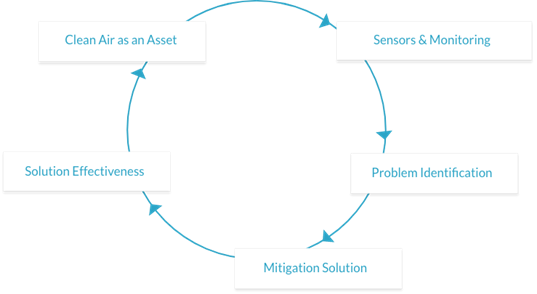
An automation and monitoring approach with software geared to be actionable is described by Qlair in a McIlvaine interview: https://youtu.be/T0HJF5MVDU0. Additional information is shown on a July 22 video https://www.youtube.com/watch?v=zYSGZt2g9KI&t=4s
Using this approach we can draw tentative conclusions. We can use generalizations about the percent of virus generated by coughs and then aerosolized. Cloth masks become aerosol generators. Cough droplets on the inner surface evaporate and then aerosols exit the mask. We assume a situation where 60% of the virus is transmitted through coughing and sneezing and 20% by contact and another 20% by aerosols.
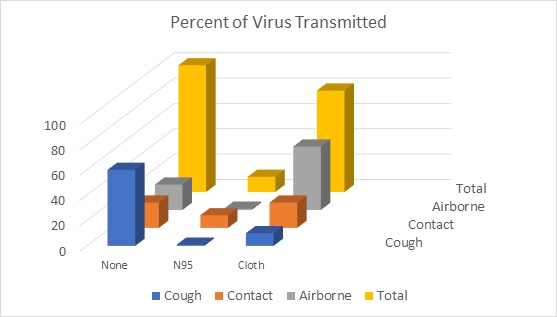
As shown in the above graph the cloth mask reduces the risk of transmission by coughing and sneezing but greatly increases the risk of airborne transmission. Logic and experimental data support this conclusion. But if true why has wearing of cloth masks reduced infections where it is being practiced. One answer is that people who wear masks are also practicing social distancing and other beneficial tactics.
The other answer is that the cloth masks prevent people from receiving sudden surges of millions of droplets and instead spread viruses out in a diluted form. Could it be that the reason the number of asymptomatic and other unreported cases is ten times higher than reported cases is due to the dilution effect of cloth masks.
Could cloth masks be unintendedly immunizing people by transmitting dilute virus quantities to them? Instead of sneezing on one person the transmitter is sending a cloud of virus in diluted numbers throughout the area. Before getting too excited about this possibility let’s heed the warning of some researchers who are worried that the small aerosols penetrate the lungs and cause more serious illness than large droplets landing the nasal passages.
The facts are that an efficient mask e.g. N95 is much safer. Mask efficiency should therefore be one of the important parameters in the UCSD collision rate model
qlAir uses CO2 as one measure of people in a space (a version of social distancing). It also can use software which will identify the numbers of people in an area served by an independent HVAC system. This means that output can be delivered using the theory with real time data.
Particulate measurements can be used as a surrogate for viral reduction. Let’s say the HVAC filter cleans the air to where the particulate in the recirculating air is only 20% of the outside air. Therefore it can be assumed that 80% of the virus has also been eliminated.
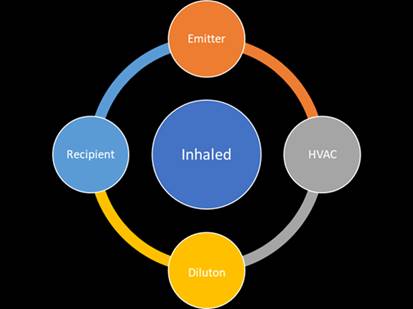
The virus transmission is a function of the amount of virus potentially exhaled by transmitters and the amount inhaled by the recipient.
|
Factor |
Relevance |
|
Number of people in HVAC area |
Number of transmitters |
|
Mask efficiency of the wearers |
A cloth mask will not likely prevent virus transmission |
|
Flow pattern of air |
Does it flow through an HVAC system before it reaches the recipient |
|
Efficiency of the HVAC filter |
Big difference between MERV 8 and HEPA |
|
Dilution of air |
The air changes per hour |
|
Air parameters such as humidity, temperature |
Virus life |
|
Number of people in HVAC area |
The transmitters are also the recipients. So their location and mask efficiency determines their risk |
All of this can be quantified with the sensors and software which can be supplied by companies like qlAir. Their analyses will show the difference made by efficient filters and masks.
The controlled direction of air flow is crucial. Ideally it should flow clockwise from the emitter to the HVAC system where most of the virus is removed. Then with laminar discharged air any remaining virus is greatly diluted before reaching the recipient.
 .
.
The goal should be to avoid counterclockwise flow from the emitter directly to the recipient.
Counterclockwise Flow with No Masks and Poor Air Flow
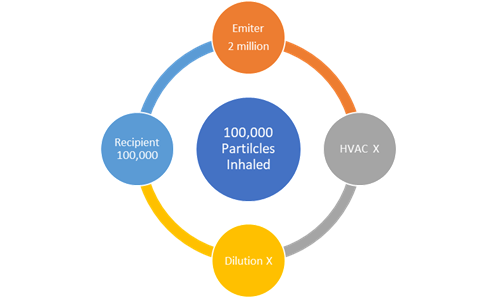
If the emitter exhales 2 million particles directly on to the recipient and neither is wearing masks the recipient could receive a very large dose. It could be as much as 100,000 particles.
Clockwise Flow with N95 Masks Good Dilution and MERV 16 Filters
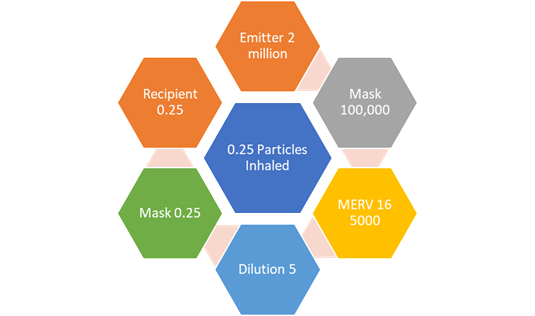
If the emitter is wearing an N95 mask and his emissions flow into the HVAC with a MERV 16 filter, the air is diluted at least by 1000 to one and the recipient is wearing an N95 mask then the recipient would receive less than one virus particle.
The proactive program, Coronavirus Technology Solutions is explained at www.mcilvainecompany.com
Bob McIlvaine can answer your questions at 847 226 2391.
Turning Off Air-Conditioning is Not a Good Idea
Jane Hu in a Slate article refuted the idea that turning off air conditioning was a solution to prevent virus spread. The Centers for Disease Control and Prevention recommends that, to prevent against airborne infections, indoor spaces should have between six and 12 full cycles of new air per hour. (Isolation units in hospitals are built to this standard.) But most buildings are only capable of one to two changes per hour, says Ed Nardell, a professor of medicine at Harvard Medical School and the Harvard T.H. Chan School of Public Health. That means airflow in these spaces is pretty minimal, with fewer chances of dispersing COVID-19 droplets.
So that might make you think that air conditioning, as the Arkansas news station said, is a terrible idea right now. But it still depends on the specific conditions of a space. In some cases it can be useful, because some airflow with air conditioning could still be better than no airflow without. “If your small enclosed room is very poorly ventilated and air just sits there for hours, air conditioning could help because you’re at least getting in that 20 percent of outdoor air and running things through some kind of filtration system,” says Linsey Marr, a professor of civil and environmental engineering at Virginia Tech who studies airborne transmission of viruses. feet.
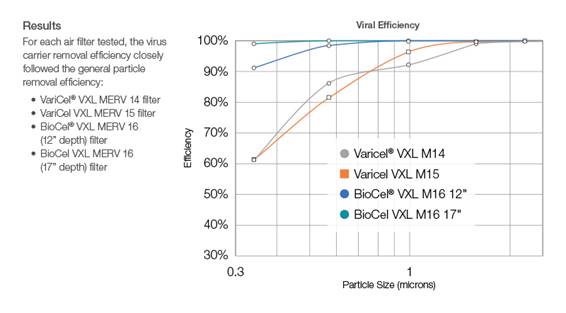
AAF Tests Efficiency of Virus Removal for Various Filters
Previous testing undertaken by a University of Minnesota research team, later replicated by AAF Flanders in their biological research laboratory at the Clean AIR Center, demonstrated that air filtration reduced not only airborne particles within the 0.5-1.0 micron size range that viruses tend to travel on, but also the virus particles themselves. For this study, the university researchers used the Porcine Reproductive Respiratory Syndrome (PRRS) Virus as the test organism for the bioaerosol tests. Because the PRRS virus studied previously is much smaller and behaves differently than the new coronavirus that causes COVID-19, AAF Flanders researchers sought answers to the question: Could a member of the coronavirus family also be filtered out of the airstream?
Because SARS-CoV-2, the coronavirus that causes COVID-19, is highly infectious to humans, the biological research team tested penetration rates for various air filters using the Porcine Epidemic Diarrhea (PED) virus as a surrogate.
Like SARS-CoV-2, the PED virus:
- Is a member of the coronavirus family
- Is of similar size
- Behaves similarly in aerosol
Fortunately, however, the PED virus is not known to infect humans, making it a safe surrogate for the AAF research trial.
Opening in 2016, the AAF Flanders Clean AIR Center (CAC) boasts 39,000 square feet of space that houses the media and materials lab, an ABSL-2 biosafety research lab, five certified ASHRAE 52.2 test ducts, and a UL-certified test duct. The unique combination of biosafety capabilities and ASHRAE test ducts positions AAF Flanders as the worldwide leader in air filtration innovation. These capabilities of the CAC make AAF Flanders the only filtration company able to replicate the University of Minnesota research that demonstrates that particle efficiency corresponds to viral removal.
AAF used essentially the same methodology as was used with the PRRS-V testing performed previously, but at higher rates of airflow (1968 CFM, as commonly used for ASHRAE 52.2 testing, rather than 650 CFM) and substituted the PED vaccine for the PRRS-V vaccine.
- First, AAF created an aerosol containing 10% Potassium Chloride (KCl), a fluorescent tracer dye to determine particle distribution by mass, and a PED vaccine with a virus concentration of 108 (or 100 million).
- The KCl was generated at particle sizes corresponding to a typical ASHRAE test size range, 0.3-10 micron, along with some larger sizes.
- That aerosol was introduced into an ASHRAE test duct and drawn through individual air filters at 1968 CFM, while keeping temperature, humidity, and other parameters at ASHRAE 52.2-prescribed levels.
- The researchers collected air samples before and after each filter with an Anderson Cascade Impactor, which separates and collects particles by size.
- They then analyzed the collected samples. First, they isolated and purified the virus in each sample. The purified virus in the samples was prepared for testing using Reverse Transcription Polymerase Chain Reaction (RTPCR) where the data generated was used to determine virus concentration per cubic meter of air. Last, AAF quantified the overall particle distribution by mass as a positive test control.
- Using this viral concentration data, AAF calculated the penetration and viral efficiency rates for each filter vs. individual particle sizes.
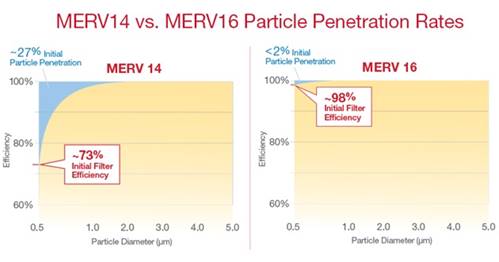
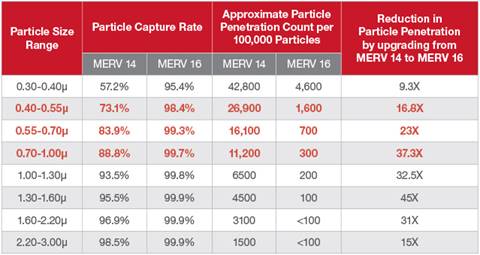
The conclusion was the percentage of airborne coronavirus-carrying particles reduced by air filtration correlates with particle efficiency.
AAF’s MERV 16 filters will not only filter out more small particles, they help minimize energy consumption, too. The BioCel® VXL box filter, for example, has initial resistance comparable to a standard box-style MERV 14 filter – allowing owners to upgrade air filtration defenses without adding significant energy costs or over-running existing system which is very stable, with no racking or vibration of the pleats under normal airflow. Pleat stability minimizes the chances of captured particulate shaking loose and re-entering the airstream.

The MERV 16 filter uses fiberglass media. Fiberglass media filters the air mechanically, without the electrostatic charge effect found in many synthetic media filters. Over time, filters made with synthetic media can lose efficiency when that charge dissipates, allowing significantly more small particles to penetrate through the filter.
Unfortunately, a filtering solution is only as strong as its weakest point. If there is not an air-tight seal between the filter and holding frame, or between holding frames, then small particles will move through the HVAC system with ease, regardless of which filter is choosen. AAF Flanders offers complimentary air filtration audits that can uncover hidden sources of dirty air bypass, as well as opportunities to realize enhanced energy efficiency and reduce strain on the HVAC equipment.