
Coronavirus Technology Solutions
July 13, 2020
A Proactive
Filtration
Industry can
Vanquish COVID
and Boost
Revenues by
Hundreds of
Billions of
Dollars
Carrier White
Paper is a Guide
to Air
Conditioning and
Ventilation to
Combat COVID
Ambrust American has Delivery Problems
Microwave can
Sterilize N95
Masks
Lots of
Decontamination
Investigations
Lysol Approved
as a
Disinfectant for
COVID
Wipes Demand
Still Exceeds
Supply
OZ Health
Contracts with
Oerlikon for
Spunbond and
Meltblown Plant
U.S. Coronavirus
Deaths Rising
and Large
Numbers are
Predicted
The Relationship
Between Viral
Load and Air
Transmission
__________________________________________________________________________
A Proactive
Filtration
Industry can
Vanquish COVID
and Boost
Revenues by
Hundreds of
Billions of
Dollars
Even though
COVID travels as
small aerosols
it is not
invincible. It
is just a matter
of choosing the
right weapons.
The filtration
industry has
developed and is
improving these
weapons. If the
filtration
industry is
proactive these
weapons will be
available in the
quantity and
time frame
needed. The
evidence
continues to
mount that
asymptomatic
individuals
transmit the
virus just by
talking or
breathing. What
is needed is to
treat the COVID
space as one big
cleanroom or one
big air
pollution stack.
Semiconductor
cleanrooms and
waste to energy
plants remove
99.99 % of
particles in the
virus size
range.
If every
transmitter and
every recipient
wore a mask as
efficient as a
cleanroom or air
pollution filter
there would not
be a problem.
Back in the
1960s the major
air pollution
source was
foundry cupolas.
There were no
national
regulations. In
fact there was
no EPA. But
States passed
regulations to
prevent the
emission of the
large particles
that fell on
nearby cars and
destroyed the
paint. So an
inefficient
device called a
multi tube
cyclone was
mandated.
It worked
well.
The big
particles were
captured and the
small particles
were invisible
and
blown
down wind
into the
next State.
A cloth face
mask is the
equivalent of
the multi tube
cyclone. It is
efficient on 100
micron particles
but captures
little below 10
microns. Today
every foundry
cupola has
efficient
filters with
nonwovens or
membranes with
efficiencies
exceeding an N95
mask. By wearing
no masks or
inefficient
masks we are
blowing the
virus downwind.
Another
challenge in
operating a
foundry cupola
is fumes which
may escape
through the
charging door.
This is solved
by good
engineering
which assures a
flow of inward
air at a
velocity
sufficient to
overcome
turbulence
within the
cupola. Air
velocity and
direction are
also important
in the
transmission of
COVID.
We used foundry
cupolas as an
example. But the
challenges in a
semiconductor or
pharmaceutical
cleanroom are
much greater and
have been met
with very robust
technology
solutions. Now
is the time for
the filtration
industry to use
its capability
and take a
proactive stance
to solve the
COVID problem.
The rewards will
be immense. The
difference
between a
reactive and
proactive
program is
hundreds of
billions of
dollars of
revenue in 2021.
With a proactive
program the air
filter and room
air purifier
sales will
increase by $60
billion per
year. Mask and
respirator sales
will increase by
over $155
billion per
year.
Disinfection,
wipes,
monitoring, and
anti-microbial
coating
revenues will
increase by over
$60 billion per
year.
In the reactive
program the
decisions are
made by
governments and
researchers. In
a proactive
program the
filtration
industry becomes
a full partner
and leader. The
position by
governments that
efficient masks
were not needed
by the public
represents a
failure by the
filtration
industry to
communicate the
basic knowledge
which it has.
This basic
knowledge has
led from the
simplistic
concept of one
large
semiconductor or
pharmaceutical
cleanroom with
all the air of
the same purity
to a concept of
many
progressively
cleaner rooms
within the main
room.
The new
classifications
are more complex
and deal with
particles of
various sizes.
The older
classification
suffices as an
illustration. It
is based on
particles 0.5
micron and
larger.
Relatively clean
ambient air is
rated at class
500,000 or
500,000
particles in
each cubic foot
of air. When a
few HEPA filters
are added you
can achieve
class 100,000.
Many
semiconductor
operators opt
for lots of
class 10,000
space with class
1 space for the
most critical
operations.
Pharmaceutical
manufacturers
opt for class
10,000 general
space with class
100 space for
vial filling
operations.
Isolators
with class 1
rating are used
for the most
critical
operations. The
COVID battle
plan can use the
same concept.
The world is one
big cleanroom in
a pyramid of
smaller spaces.
Each local space
has its own more
restrictive
efficiency
criteria and
then the
individual
represents the
smallest
cleanroom within
the pyramid.
Class 500,000:
Let’s
start with the
class 500,000
cleanroom or
ambient air. The
problem is that
the ambient air
at traffic
intersections in
the cleanest
cities and the
air throughout
many cities
and even
the rural areas
in many
countries
contains many
millions of 0.5
micron particles
per cubic foot.
This is why
Germany is
supplying
ambient air
filtration
systems at some
traffic
intersections.
This is why in
India, China,
and many other
countries
efficient masks
are worn by many
citizens.
Small air
pollution
particles are
not stopped by
cloth masks. So
there is already
a large market
for efficient
masks in many
countries. The
masks which stop
small dust
particles will
also capture the
small virus
particles. In
fact research in
the Lombardy
region in Italy
as well as other
studies show
that the virus
can be attached
to air pollution
particles.
The need to
protect against
the air
pollutants will
be there long
after a vaccine
to prevent COVID
is made
available and
will be there
until the next
virus comes
along. This
means that the
filtration
industry has the
promise of a
large and
continuing
revenue stream
in the Class
500,000 space.
The individual
is the
ultimate
cleanroom within
a cleanroom. He
can change the
cleanroom class
in the air
around him with
a mask. When he
is far from
others, he may
be safe with no
mask and willing
to breathe in
the 500,000
particles with
every cubic foot
inhaled.
Class 100,000:
Many industries
making small
parts operate in
class 100,000
cleanrooms. Food
processing
plants strive to
keep general
space at this
cleanliness
level. Pork
processing
plants have
found that the
shelf life of
their product is
increased by
more than one
week if they
have cleaner air
in the
production
facilities. The
combination of
improved HVAC
and filtration
combined with
the use of
efficient masks
would eliminate
much of the
virus
transmission
presently
occurring in
these
facilities.
Partitions
without air
control can make
matters worse
not better.
The general
space in
hospitals should
be at least
class 100,000.
Hospital
acquired
infections
result in
millions of
deaths per year.
Visitors
account
for some of this
transmission.
PathO3Gen
Solutions found
that their foot
sanitizer used
by all those
entering a
hospital makes a
big difference.
Train stations,
airline
terminals,
nursing homes,
apartment
complexes,
office buildings
and other areas
of congregation
should be kept
in this class
range. The air
in many office
buildings
contains VOCs
generated from
plastic
furniture, floor
coverings etc.
Efficient masks
are needed in
these areas but
in addition
relatively pure
air should be
provided.
An N30 mask will
insure
maintenance of a
class 100,000
atmosphere but
in situations
where people
congregate the
individual
should convert
his inhaled air
to class 100
with an N95
mask.
Class 10,000:
There
have been
initiatives to
eliminate
pharmaceutical
and
semiconductor
class 10,000
space.
Since
people generate
the
contamination,
the concept was
to use isolators
and robotics and
keep people out
of the
production
space. In
practice some
human
intervention is
necessary and no
matter how well
sealed a class l
cleanroom is it
helps if it is
surrounded by
relatively clean
air.
This principle
can be applied
to COVID. Luxury
hotels are
willing
to spend lots of
money to make
their
accommodations
safe. In
addition to
requiring guests
to wear masks it
can create
general space
with class
100,000 air
purity.
Elevators, gyms,
and restrooms
can be designed
as
class
10,000 space.
In the case of
an individual
you have a
twostep process
Step 1 is
filtering out
viruses being
transmitted.
Step 2 is
filtering out
viruses being
inhaled.
Step 1 can be
the filter in an
HVAC system or
it can be a
mask. In each
case the amount
of virus inhaled
is a function of
the combined
efficiency
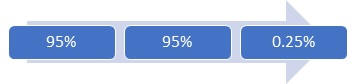
For example if
the transmitter
and recipient
each have N95
masks then the
virus inhaled by
the recipient is
only 0.25
percent.
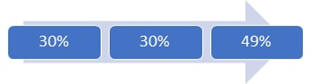
Compare
this to the N30
mask where the
combination
results in the
recipient
inhaling 49
percent of the
virus.
A MERV
13 filter in an
HVAC system can
provide a 30
percent
reduction in
viruses or
equivalent to an
N30 Mask. So if
you have a
building with
MERV 13 filters
providing 10 or
more air changes
per hour to each
space and if
each transmitter
and recipient
wears N30 masks
the virus
level is
reduced
in three steps.
Seventy percent
is reduced in
the first step
another 21
percent reduced
in the second
step and another
15 percent in
the third step
leaving 35
percent of the
virus to be
inhaled.
Let’s take the
example of a
hotel elevator
with a HEPA
filter
delivering class
10,000 air. The
transmitter
rides to his
floor but is
wearing an N30
mask
So the
elevator air
contains only 70
percent of the
virus from the
transmitter. The
elevator HVAC
system removes
95 percent of
the virus
leaving only 3.5
percent in the
elevator when
the recipient
enters. He is
wearing an N30
mask so he
inhales only 1.2
percent of the
potential
transmission.
If a HEPA filter
is installed in
a robust HVAC
system and
laminar air flow
prevents the
transmitter from
directly
exhaling to the
recipient then
99 percent of
the virus is
captured even if
the recipient
has no mask. In
reality it is
prohibitively
expensive to
create a space
with the ceiling
covered with
HEPA filters
discharging at
100 fpm and air
return systems
below a
perforated
floor. So some
air will flow
from transmitter
to recipient
without being
first filtered.
So the recipient
will be
contaminated by
the general
viral load plus
any virus
from a
transmitter
circumventing
the HVAC system.
Class 1000 to
Class 1: Drug
preparation
areas of
hospitals are
often designed
for class 1000
but with class
100 enclosures
around actual
filling
operations.
Isolation rooms
in hospitals are
designed to be
class 100 but
also to be under
negative
pressure.
The decision to
invest in a
class 10 or
class 1 space is
a function of
risks to
products or
people. When
applying
this to
COVID it is a
consideration of
risk to the
general
population as
opposed to the
risks to a
specific
individual. N30
masks may be
sufficient to
reduce the
number of cases
in the general
population. But
if the new cases
are 100 today
and 99 tomorrow
it is not
positive news
for the 99. If
by wearing N95
masks the new
cases drop from
100 to 5 this is
very positive
for 95
individuals.
The weapons to
fight COVID are
reduced levels
of virus in the
local space plus
reduction from
individual
transmitters and
efficient
elimination of
viruses by the
inhaling
recipient. Every
cleanroom
operator would
prefer to
operate in a
class 1 space
but the cost
exceeds the
value in most
cases. So there
is always a
risk. Whether it
is
pharmaceutical
products, chips,
or individuals
the risk and
rewards need to
be analyzed and
the proper level
of investment
made.
Information on Coronavirus Technology Solutions is found at: http://home.mcilvainecompany.com/index.php/markets/air/82ai-coronavirus-market-intelligence
Information on
relevant market
reports is found
at
www.mcilvainecompany.com
and then
click on
markets.
Carrier White
Paper is a Guide
to Air
Conditioning and
Ventilation to
Combat COVID
Carrier has published a white paper
relative to
COVID and
air
conditioning. It
reviews
the Chinese
restaurant
incident which
has been covered
in previous
Alerts. It makes
the point that
air distribution
was the culprit
and not the use
of AC. It
cites no
trace of virus
on the AC
duct. On
the other hand
other studies
show deposits in
HVAC systems. In
fact Carrier has
anti-microbial
coatings
for duct
interiors. Also
since Carrier is
now offering
HEPA filtered
room air
purifiers for
schools and
other gathering
places, the
value of high
efficiency
filtration is
communicated.
Here is a
summary and link
to the white
paper.
ASHRAE guidelines point to an upper limit
of air velocity
in the occupied
space of 40 fpm.
To achieve this
condition, the
air needs to be
properly blown
by the HVAC
system into the
room, and
properly
distributed in
the occupied
space.
A generation of research and experience
has proven that
when properly
maintained and
operated,
heating,
ventilation and
air-conditioning
systems (HVAC)
can reduce the
spread of
viruses. These
critical
building systems
not only provide
thermal comfort
but, according
to the American
Society of
Heating,
Refrigerating
and Air
Conditioning
Engineers
(ASHRAE), may
also improve
resistance to
infection.
HVAC systems work in a built environment
to supply
comfortable,
clean,
recaptured air,
mix in healthy
levels of fresh
air, and contain
or exhaust
contaminants.
Air delivery
systems can
reduce the
transmission of
viruses through
inline
filtration,
something HVAC
professionals
are capable of
assessing.
Air-conditioning
systems are also
critical in
maintaining
healthy humidity
levels.
“Maintaining a
RH (relative
humidity)
between 40% and
60% indoors may
help to limit
the spread and
survival of
SARS-CoV-2
within the BE,”
the ASM
suggests, “while
minimizing the
risk of mold
growth and
maintaining
hydrated and
intact mucosal
barriers of
human
occupants.” The
Centers for
Disease Control
(CDC) echoes
these findings,
saying that
employers can
decrease the
spread of
COVID-19 by
maintaining a
healthy work
environment.
“Consider
improving and
engineering
controls using
the building
ventilation
system,” the CDC
suggests,
including
increased
ventilation
rates and
increased
percentage of
outdoor air
circulating
through the
system. Well
before COVID-19,
the Healthy
Building
Movement had
begun to measure
and improve air
quality in the
built
environment to
improve
productivity and
health. Of the
nine foundations
for a healthy
building, five
relate to HVAC,
including air
quality,
ventilation,
thermal health,
moisture, dust
and pests.
“There’s just no
reason anymore
to economize on
airflow and
filtration,”
Harvard Business
School’s John
Macomber says.
“It’s a cheap
way to help
people be
healthier.
To ensure the proper indoor air purity, a
good HVAC system
should include
some or all of
the following:
1. (Demand Controlled) Ventilation: When
outside air is
not provided via
separate
devices, the
HVAC system
should provide
outside air
based on the
size/use of the
space. Where
possible, the
HVAC system
should include a
sensor for
carbon dioxide
or other
pollutants to
calculate and
correct in real
time the amount
of ventilation
needed. It is
important to be
aware that the
increase of the
ventilation rate
may cause an
increase of
load, and the
HVAC unit, if
not properly
sized, may not
be able to
provide
sufficient
cooling
capacity. In
such situations,
it may be
appropriate to
consider Direct
Outdoor Air
Supply (DOAS)
units, which are
specifically
designed for
large amounts of
outside air.
2.
Filtration:
Filters are
rated on their
ability to
capture and
retain particles
of different
sizes. The
industry
standard is a
Minimum
Efficiency
Reporting Value
(MERV) rating.
Filters with
MERV >13 have a
significant
ability to
capture
particulate
matter (PM) and
smaller
particles. HEPA
filters are even
more efficient
and are able to
capture bacteria
and viruses.
Note that there
are important
tradeoffs to
consider: the
higher the
filtration
requirements,
the greater the
air pressure
drop and the
size of the
filter. For this
reason, the air
management
system of the
HVAC needs to be
carefully sized
based on the
filtration
requirements.
3. Other Indoor Air Quality Devices:
Numerous
technologies are
available to
reduce the
presence of
contaminants.
Ultraviolet
lights,
ultraviolet
photocatalytic
oxidation,
ionization,
plasma,
electrostatic
active, active
carbon and other
components can
be installed to
specifically
target volatile
organic
compounds (VOC),
bacteria and
viruses. Some of
these options
can be available
as integral
parts of the
HVAC system.
https://www.shareddocs.com/hvac/docs/1001/Public/02/COVID-19-WHITE-PAPER.pdf
Ambrust American has Delivery Problems
Friday, we reported on the big Texas
school order for
the company. The
company has also
offered masks to
the public but
had
delivery
problems.
Lloyd Armbrust,
the founder
said, “ we set
up a website
really fast, and
we just made so
many mistakes.”
Armbrust tells
KXAN there were
logistical and
technical
problems that
led to shipping
delays. That’s
in addition to
the large number
of orders the
company received
for masks.
Armbrust says
he set an order
limit of one
purchase per
customer, but
not on the total
volume of orders
received. The
company received
1.6 million
orders in the
week after the
KXAN
story
aired.
In a sense,
Armbrust
American began
suffering from
its own success.
“I didn’t
really
appreciate the
amount of effort
that it takes
for something to
arrive magically
on my doorstep,”
he said.
Bonnie Bryce
was one of the
customers who
watched the
story, and
ordered 50 masks
from the
company.
“I’m 67 years
old and I had
heart surgery in
February,” she
told us over the
phone Tuesday.
“So my
cardiologist
advised me to be
diligent about
wearing a mask.”
After placing
her order on May
20, she received
a confirmation
email, but
nothing after
that.
Many customers
have found
themselves in a
similar
situation. KXAN
received a
number of
concerns from
people, asking
about the
company and when
they would get
their masks.
Still more
people reached
out to Armbrust
American
directly. We
found a number
of negative
reviews and
posts about the
delays on social
media.
“I thought
maybe he got
overwhelmed a
little bit,”
said Bryce.
After our
interview
Tuesday,
Armbrust
informed us that
Bryce’s order
was shipped,
with a few extra
masks thrown in.
Ultimately,
millions of
masks had been
sitting in the
factory the
entire time.
The company’s
automated
machines can
make 100 masks a
minute. The
delays instead
came with
packing, sealing
and shipping.
Armbrust
explained that
automated
machines cannot
seal and pack
the masks
without bending
them. Therefore,
people have to
do it.
He says it
used to take 10
minutes to box
up 50 masks, but
the company is
now able to do
it in 30
seconds.
Armbrust says
the original
promise was to
ship the masks
to customers one
week after
they’d placed
the order.
He realized
quickly he
wouldn’t be able
to make that
deadline, due to
the huge demand.
He says he sent
a video out to customers explaining
the situation
late last month
but believes
many people
didn’t get the
message.
“I think the
lesson is, when
you start a
company, you
need to make
sure you have
your supply
chain ironed out
before you go on
television,”
said Bryce.
Armbrust
agrees.
“I’d say the
biggest thing I
learned was
setting the
proper
expectations for
people, and to
really
understand the
entire picture,”
he said.
The company is
trying to catch
up now. Armbrust
says he is
prioritizing
orders for
healthcare
workers and
people more
vulnerable to
COVID-19, which
is caused by the
coronavirus.
He added that
all orders out
of Texas would
be shipped out
this week, but
also understands
if people cancel
their order.
Over the last
couple of weeks,
the only option
has been to
pre-order masks,
while the
company catches
up. Those orders
were to go out
starting July 1.
Microwave can
Sterilize N95
Masks
A recent
study from
the American
Society for
Microbiology
offers a new
decontamination
tool that is
much more
accessible and
affordable: a
microwave. Researcher James E. Kirby, MD, from the Beth
Israel Deaconess
Medical Center
of Harvard says
the study’s
findings are
crucial to the
many health care
centers that
lack the
high-capacity
sterilization
systems of large
hospitals.
“We knew there was a critical shortage of personal
protective gear
and N95 masks,
and we knew
there was a need
for a solution,”
he says.
The team of eight researchers set out to provide
an easy
disinfection
method to
different health
care settings
including
“outpatient
practices,
frontline
providers, and
remote clinical
settings.”
“The goal of this work was to identify a widely
accessible,
microwave-generated
steam
decontamination
method,” the
article says.
“To this effect,
we utilized only
common household
items.”
The materials include water, a glass container,
mesh, a rubber
band, and a
1,100- or
1,150-watt
microwave. The
researchers
filled the
container with
60 milliliters
of water, then
secured the mesh
material over
the top of it
with a rubber
band. They then
placed the N95
mask on the mesh
and microwaved
it for 3
minutes. This
effectively
killed all
viruses,
including
coronavirus,
they say.
“It’s simple, but sometimes very simple things
work well,”
Kirby says.
The researchers found that this sterilization
method could be
repeated 20
times on a
single N95 mask
without
damage. Even
though the type
of mask they
used had a metal
piece, they
didn’t have an
issue with it
heating or
sparking during
the 20 cycles of
testing, Kirby
said.
Though the study was done with health care
settings in
mind, Kirby
doesn’t see the
harm in trying
the same method
at home.
A recent USA
Today opinion
piece by
ICU specialists
Pierre Kory, MD,
and Paul H.
Mayo, MD,
reinforces the
importance of
N95s as
coronavirus
rates increase.
Their stance is
grounded on
emerging
evidence showing
that coronavirus
may be
transmitted via
aerosol
droplets.
“The only mask that can prevent aerosol-size
droplet
inhalation is an
N95,” the
authors say.
Due to the shortage of N95s available to health
care workers,
many people are
wearing cloth
masks, which can
be
decontaminated
in the washer.
But more people
may turn to N95
masks as more
research emerges
about the pandemic’s transmission.
Lots of
Decontamination
Investigations
Bloomberg has
summarized a
number of
investigations
into mask
decontamination.
Richard Peltier,
an aerosol
chemist and
associate
professor at the
University of
Massachusetts-Amherst,
is researching
the
effectiveness of
different
decontamination
methods and how
many cycles a
mask can go
through before
its filtering
abilities drop
below the N95
respirator’s
required
threshold. The
research is
funded by the
National Science
Foundation.
To meet the
government’s N95
designation, a
mask must filter
out at least 95%
of particles
that are 300
nanometers or
larger—enough to
trap a single
coronavirus.
Peltier said he
first started
looking at
whether a
decontaminated
N95 mask
continued to be
effective at the
request of a
local hospital
that was
considering
exposing masks
to a
gas—vaporized
hydrogen
peroxide—a
process often
used to
sterilize
medical
equipment.
Using a device
that measures
whether an N95
mask is
filtering out
the microscopic
particles,
Peltier said he
confirmed the
mask was still
functioning
after one
decontamination
cycle.
That led to the
NSF project
where Peltier
evaluated masks
that had gone
through the
vaporized
hydrogen
peroxide process
or several other
decontamination
methods through
up to 10 cycles.
The study is
undergoing peer
review, Peltier
said, and he
can’t yet
discuss his
conclusions.
However, he did
say some
sterilization
methods did
lower masks’
effectiveness
below the N95
threshold.
Companies
manufacturing
N95 respirators
and performing
the
decontamination
work also have
been looking at
the
effectiveness of
N95 masks after
multiple
sterilizations.
Dr. Nikki
McCullough, a
health and
occupational
safety leader in
3M’s Personal
Safety Division,
said 3M has
evaluated some
of its masks
after
decontamination
to determine
through how many
cycles a mask
stays effective.
3M has approved
masks going
through up to 20
cycles. The
limits are
updated
regularly in a bulletin 3M
publishes.
McCullough
cautioned that
other factors
must be
considered on
whether a mask
is still
protective. “The
number of cycles
that a
particular
respirator will
withstand will
depend on how
many times it
has been donned,
stored and
duration and
conditions of
use,” she said.
If a user can’t
get the mask to
form a proper
seal on the
user’s face, the
mask shouldn’t
be worn,
McCullough said.
The Centers for
Disease Control
and Prevention
published guidance for
the maximum
number of times
N95 masks can be
sterilized using
a wide range of
methods from
steam heat
generated inside
a microwave oven
to exposing the
masks to
ultraviolet
light.
The largest
decontamination
effort is
overseen by
Battelle
Memorial
Institute, an
Ohio nonprofit
company.
Will Richter, a
microbiologist
and principal
research
scientist with
Battelle, said
the company has
decontaminated
about 1.2
million N95
masks at centers
across the
nation.
In April,
Battelle was
awarded a
contract from
the Defense
Department,
worth up to $415
million, to open
and operate 60
decontamination
centers that
would sterilize
respirators sent
by health-care
providers.
Richter said
Battelle found
that 20
different models
of N95 mask, and
10 foreign-made
masks, remain
effective
through 20
cycles. The
company has also
cooperated with
3M and the CDC’s
National
Institute for
Occupational
Safety and
Health to
evaluate the
Battelle system.
Battelle’s
systems use
vaporized
hydrogen
peroxide. Each
system can
sterilize about
5,000 masks at a
time in a
process that
takes about 24
hours, Richter
said.
While the CDC
has approved
Battelle’s
methods for up
to 20
sterilization
cycles, Richter
said, the
company has its
own quality
controls. Masks
that are
stained, often
from makeup, or
otherwise appear
soiled, aren’t
processed. Also
pulled out are
masks with
apparent
material flaws
such as broken
straps.
After a batch of
masks has been
decontaminated
and “air washed”
to allow
residual gas to
dissipate,
workers use gas
detectors to
determine if the
amount of
hydrogen
peroxide gas is
below the OSHA
permissible
exposure limit,
Richter said.
The OSHA limit
is 1.0 parts per
million, but
Battelle
enforces a
stricter limit,
0.8 parts per
million.
Of the 1.2
million masks
Battelle has
processed and
returned, the
company has
received
complaints about
fewer than 0.5%
of the masks,
Richter said.
https://news.bloomberglaw.com/safety/decontaminating-covid-19-masks-raises-safety-efficacy-concerns
Lysol Approved
as a
Disinfectant for
COVID
Lysol is the
first surface
disinfectant
approved by the
Environmental
Protection
Agency to wipe
out the
coronavirus.
Two versions of
the common
household
disinfectant
spray were lab
tested by the
agency, which
found they could
kill the virus
on surfaces, the
EPA
announced. Lysol
Disinfectant
Spray, priced
at $4.18 at
Walmart,
and Lysol
Disinfectant Max
Cover Mist, priced
at $5.48,
can kill the
virus in under 2
minutes, the
agency found.
"The EPA's
approval
recognizes that
using Lysol
Disinfectant
Spray can help
to prevent the
spread of
COVID-19 on
hard, non-porous
surfaces," said
Rahul
Kadyan, executive
vice president
of hygiene for
Lysol's parent
company Reckitt
Benckiser in a
statement.
"In the face of
the pandemic,
Lysol continues
to work with a
wide range of
scientific and
health experts
to educate the
public on the
importance of
hygiene.
In March, the
EPA released a lengthy list of
household
cleaners that
were expected to
be effective
against
coronavirus
because they
have been tested
and proven to
work against
similar viruses.
The news sent
the products
flying off
shelves, leading
to shortages at
many local
grocery stores.
Many
supermarkets
still limit the
number of
cleaning
supplies people
can buy to cut
down on
hoarding. Supply
chain experts
previously told
USA TODAY that manufacturers like Lysol and Clorox weren't ready for
a flood of
Americans
suddenly
shopping for
disinfectant.
Wipes Demand
Still Exceeds
Supply
“This is
unprecedented
demand in modern
times for
products like
disinfecting
wipes,” says
Brian Sansoni,
senior vice
president,
Communications,
Outreach &
Membership for The
American
Cleaning
Institute (ACI),
a U.S.-based
trade
association for
the cleaning
products
industry.
“Manufacturers
have been
working around
the clock as
they are able to
get as many
workers in
there—working
safely as well,
as the safety of
the workforce is
paramount.”
Based on reports
and analysis
from
manufacturers,
the ACI
estimates that
consumers will
begin to see a
more regular
supply of
products like
disinfectant
wipes in
mid-summer.
Major
manufacturers of
disinfectants
and disinfectant
wipes weren’t
quite prepared
for such high
demand this time
of year.
On The
Clorox Company’s
earnings call
last month,
chairman and CEO
Benno Dorer
reported that
the company had
all-time record
shipments of
Clorox
disinfecting
wipes, cleanup
disinfecting
spray,
disinfecting
bathroom cleaner
and Scentiva
products. Demand
for some
disinfectant
products spiked
more than 500%.
“Demand has been
clearly
unprecedented,”
he said.
Dorer told
analysts that
the company has
been able to
increase
production of
disinfecting
products by 40%.
It’s now
focusing on
fewer SKUs;
production of
its line of
Clorox
compostable
cleaning wipes
is on hold for
now in order to
prioritize
disinfecting
wipes.
Clorox has also
activated
third-party
suppliers to
help it cope
with the surge
in demand. “We
continue to find
new ways to
increase our
capacity,” he
added.
In terms of
availability,
Dorer told
Yahoo! Finance
last month that
there will be
substantial
improvements in
supply this
summer. “It’s
going to be
touch and go
until then,
unfortunately.
But help is on
the way, and I
think things
should ease up
in the next few
months
To alleviate
shortages caused
by consumer
stockpiling,
wipes
manufacturers
have been
working as
quickly and
safely as
possible to
crank up
capacity.
“Companies
certainly ramped
up production to
meet the demand,
while retailers
have been
seeking to
normalize the
supply situation
by restricting
purchases per
customer,” says
Svetlana
Uduslivaia, head
of Home and Tech
Americas at
Euromonitor
International.
“As stay-at-home
restrictions
ease and some of
the at-home
consumption
normalizes,
coupled with
ramped up
production, the
situation will
likely normalize
in retail.”
OZ Health
Contracts with
Oerlikon for
Spunbond and
Meltblown Plant
OZ Health Plus
will establish
Australia’s
first
manufacturing
plant to make
the critical
fine plastic
material used in
most protective
face masks. OZ
Health Plus has
purchased a
plant of the
Swiss-based
technology
company Oerlikon to
establish a
Queensland-based
production plant
for spunbond and
meltblown
nonwovens. These
fabrics are
essential for
Australia’s face
mask
manufacturers,
who currently
produce about
500 million
medical and
industrial masks
per year.
However the
fabrics have to
be imported from
overseas and
access to these
materials has
been severely
disrupted during
the COVID-19
pandemic.
Oerlikon’s
German-based
business unit
Oerlikon
Nonwoven has now
executed legal
and commercial
arrangements to
supply the
specialized
machinery which
can manufacture
the nonwoven
material
locally. The
same machinery
is used to make
almost all face
masks material
manufactured in
Europe. The
world-leading
Oerlikon
Nonwoven
meltblown plant
will commence
operations in
April next year,
with a second
stage planned
for late 2021.
The Oerlikon
Nonwoven plant
can produce
meltblown
fabrics for 500
million masks
per year, along
with other
medical and
non-medical
grade products,
filtration
products,
sanitary items,
antiseptic wipes
and more. Rainer
Straub, head of
Oerlikon
Nonwoven, says:
“We are very
proud that we
can now for the
first time
supply our
Oerlikon
Nonwoven
meltblown
technology to
Australia. Due
to the short
delivery time,
we hope to make
our contribution
to the
Australian
population and
their safe
supply of
high-quality
protective masks
as soon as
possible.”
OZ Health Plus
director Darren
Fooks says:
“Australia has
access to raw
polypropylene
feedstock but
lacks the plant
to convert that
raw material to
specialized
spunbond and
meltblown
fabrics. These
fabrics are
essential for
local mask
manufacturing.
The Australian-
based Oerlikon
Nonwoven plant
will fill the
production chain
gap for
Australia by
producing the
fabrics we need
for mask
production and
many other
products – it
will reduce
Australia’s
protective mask
supply chain
from thousands
of kilometers,
to tens of
kilometers.”
“Our decision in
favor of
Oerlikon
Nonwoven was a
given once we
had analyzed the
material
samples. It was
a matter of
course for us
that the
Business Unit of
the Oerlikon
Manmade Fibers
segment could
supply
high-quality
machines and
systems,” adds
Fooks.
OZ Health Plus’
new facilities
will take up
15,000 m2 of
manufacturing
space and will
employ 100
full-time roles
once the second
stage of the
project is
complete. OZ
Health Plus
continues to
work with both
Queensland and
Federal
Government
stakeholders and
values their
support in
bringing this
vital capability
to Queensland.
U.S. Coronavirus
Deaths Rising
and Large
Numbers are
Predicted
A long-expected
upturn in U.S.
coronavirus
deaths has
begun, driven by
fatalities in
states in the
South and West,
according to
data on the
pandemic.
The number of
deaths per day
from the virus
had been falling
for months, and
even remained
down as states
like Florida and
Texas saw
explosions in
cases and
hospitalizations
— and reported
daily U.S.
infections broke
records several
times in recent
days.
Scientists
warned it
wouldn’t last. A
coronavirus
death, when it
occurs,
typically comes
several weeks
after a person
is first
infected. And
experts
predicted states
that saw
increases in
cases and
hospitalizations
would, at some
point, see
deaths rise too.
Now that’s
happening.
“It’s
consistently
picking up. And
it’s picking up
at the time
you’d expect it
to,” said
William Hanage,
a Harvard
University
infectious
diseases
researcher.
According to an
Associated Press
analysis of data
from Johns
Hopkins
University, the
seven-day
rolling average
for daily
reported deaths
in the U.S. has
increased from
578 two weeks
ago to 664 on
July 10 — still
well below the
heights hit in
April. Daily
reported deaths
increased in 27
states over that
time period, but
the majority of
those states are
averaging under
15 new deaths
per day. A
smaller group of
states has been
driving the
nationwide
increase in
deaths.
California is
averaging 91
reported deaths
per day while
Texas is close
behind with 66,
but Florida,
Arizona,
Illinois, New
Jersey and South
Carolina also
saw sizable
rises. New
Jersey’s recent
jump is thought
to be partially
attributable to
its less
frequent
reporting of
probable deaths.
The virus has
killed more than
130,000 people
in the U.S. and
more than a
half-million
worldwide,
according to
Johns Hopkins
University,
though the true
numbers are
believed to be
higher.
Deaths first
began mounting
in the U.S. in
March. About two
dozen deaths
were being
reported daily
in the middle of
that month. By
late in the
month, hundreds
were being
reported each
day, and in
April thousands.
Most happened in
New York, New
Jersey and
elsewhere in the
Northeast.
Deaths were so
high there
because it was a
new virus
tearing through
a densely
populated area,
and it quickly
swept through
vulnerable
groups of people
in nursing homes
and other
places, said
Perry Halkitis,
the dean of the
Rutgers
University
School of Public
Health in New
Jersey.
Many of the
infections
occurred before
government
officials
imposed
stay-at-home
orders and other
social-distancing
measures. The
daily death toll
started falling
in mid-April —
and continued to
fall until about
a week ago.
Researchers now
expect deaths to
rise for at
least some
weeks, but some
think the count
probably will
not go up as
dramatically as
it did in the
spring — for
several reasons.
First, testing
was extremely
limited early in
the pandemic,
and it’s become
clear that
unrecognized
infections were
spreading on
subways, in
nursing homes
and in other
public places
before anyone
knew exactly
what was going
on. Now testing
is more
widespread, and
the magnitude of
outbreaks is
becoming better
understood.
Second, many
people’s health
behaviors have
changed, with
mask-wearing
becoming more
common in some
places. Although
there is no
vaccine yet,
hospitals are
also getting
better at
treating
patients.
Another factor,
tragically, is
that deadly new
viruses often
tear through
vulnerable
populations
first, such as
the elderly and
people already
weakened by
other health
conditions. That
means that, in
the Northeast at
least, “many of
the vulnerable
people have
already died,”
Halkitis said.
Now, the U.S. is
likely in for “a
much longer,
slower burn,”
Hanage, the
Harvard
researcher,
said. “We’re not
going to see as
many deaths (as
in the spring).
But we’re going
to see a total
number of
deaths, which is
going to be
large.”
The Relationship
Between Viral
Load and Air
Transmission
According to MIT
one of the
biggest
questions we
still have about
covid-19 is how
much of a viral
load is needed
to cause
infection. The
answer changes
if we think it
is aerosols that
we need to worry
about. Smaller
particles won’t
carry as large a
viral load as
bigger ones, but
because they can
linger in the
air for much
longer, it may
not
matter—they’ll
build up in
larger
concentrations
and get
distributed more
widely the
longer an
infected person
is around to
expel
aerosolized
virus.
The more people
you have coming
in and out of an
indoor space,
the more likely
it is that
someone who is
infected will
show up. The
longer those
infected
individuals
spend in that
space, the
higher the
concentration of
virus in the air
over time. This
is particularly
bad news for
spaces where
people
congregate for
hours on end,
like
restaurants,
bars, offices,
classrooms, and
churches.
Airborne
transmission
doesn’t
necessarily mean
these places
must stay closed
(although that
would be ideal).
But wiping down
surfaces with
disinfectant,
and having
everyone wear
masks, won’t be
enough. To
safely reopen,
these spots will
not just need to
reduce the
number of people
allowed inside
at any given
moment; they
will also need
to reduce the
amount of time
those people
spend there.
Increasing
social
distancing
beyond six feet
would also help
keep people
safer.
Ventilation
needs to be a
higher priority
too. This is
going to be a
big problem for
older buildings
that usually
have worse
ventilation
systems, and
areas with a lot
of those might
need to remain
closed for much
longer. The
impact of asymptomatic spread (transmission
by people who
don’t feel ill)
and superspreaders only
compounds the
problem even
further. But research conducted by the US
Department of
Homeland
Security has
shown that in
the presence of
UV light,
aerosolized
particles of the
size the Tulane
researchers
studied would
disappear in
less than a
minute. A number of businesses have
begun deploying
UV-armed robots
to disinfect
hospital rooms,
shopping malls,
stores, public
transit
stations, and
more.
For many places,
considerable
delays in
economic
reopening might
ultimately be
the price of
getting the
virus under
control.
Otherwise the
kind of thing
that happened
when a single
open bar in
Michigan led
to an outbreak
of more than 170
new cases could
become
commonplace.
This article in
the MIT
Review also
documents the
evidence that
the virus is
airborne and
points out that
inefficient
masks which are
not tight
fitting are not
going to prevent
transmission of
these small
aerosols.
The
authors
therefore
recommend
distancing and
other
non-filtration
initiatives.
McIlvaine
asks the
question why
doesn’t everyone
just wear a mask
which will
capture these
small particles?
