
Coronavirus Technology Solutions
June 16, 2020
Elastomeric Masks
are the Choice for AHN
UV Sterilization does not Impact Mask Efficiency
According to ASU Studies
Ultraviolet
Sanitization Kit for Masks, Wallets, Keys and
Glasses
North Carolina Meat and Poultry Industry has
Major COVID Problem
Social Distancing is not a Safe Solution
____________________________________________________________________________
Elastomeric Masks
are the Choice for AHN
A cost-effective strategy for health care
systems to offset N95 mask shortages due to the
Coronavirus Disease 2019 (COVID-19) pandemic is
to switch to reusable elastomeric respirator
masks, according to new study results. These
long-lasting masks, often used in industry and
construction, cost at least 10 times less per
month than disinfecting and reusing N95 masks
meant to be for single use, say authors of the
study, published as an "article in press" on
the Journal of the American College of
Surgeons website in advance of print.
The study is one of the first to evaluate the
cost-effectiveness of using elastomeric masks in
a health care setting during the COVID-19
pandemic, said Sricharan Chalikonda, MD, MHA,
FACS, lead study author and chief medical
operations officer for Pittsburgh-based
Allegheny Health Network (AHN), where the study
took place.
Disposable N95 masks are the standard face
covering when health care providers require
high-level respiratory protection, but during
the pandemic, providers experienced widespread
supply chain shortages and price increases, Dr.
Chalikonda said. He said hospitals need a
long-term solution.
"We don't know if there will be a shortage of
N95s again. We don't know how long the pandemic
will last and how often there will be virus
surges," he said. "We believe now is the time to
invest in an elastomeric mask program."
Dr. Chalikonda said an immediate supply of
elastomeric masks in a health care system's
stockpile of personal protective equipment is
"game changing" given the advantages.
Elastomeric masks are made of a tight-fitting,
flexible, rubber-like material that can adjust
to nearly all individuals' faces and can
withstand multiple cleanings, Dr. Chalikonda
said. These devices, which resemble gas masks,
use a replaceable filter. According to the
Centers for Disease Control and Prevention
(CDC), elastomeric masks offer health care
workers equal or better protection from airborne
infectious substances compared with N95 masks.
Like many hospitals during the COVID-19 crisis,
AHN was disinfecting and reusing N95 masks for a
limited number of uses. However, Dr. Chalikonda
said, "Many caregivers felt the N95 masks didn't
fit quite as well after disinfection."
At the end of March, AHN began a one-month trial
of a half-facepiece elastomeric mask covering
the nose and mouth. The mask holds a P100-rated
cartridge filter, meaning it filters out almost
100 percent of airborne particles.
Until AHN could procure more elastomeric masks,
the system began its program for P100
elastomeric mask "super-users": those providers
who have the most frequent contact with COVID-19
patients. At each of AHN's nine hospitals in
Pennsylvania and Western New York, the first
providers to receive the new masks were
respiratory therapists, anesthesia providers,
and emergency department and intensive care unit
(ICU) doctors and nurses. Initially, providers
shared the reusable masks with workers on other
shifts, and the masks underwent decontamination
between shifts using vaporized hydrogen peroxide
similar to the technique used to sterilize
disposable N95 masks.
Another advantage of an elastomeric respirator
program, according to Dr. Chalikonda, is it does
not require any additional hospital resources to
implement if the hospital already has an N95
mask reuse and resteriliation program. The AHN
elastomeric mask program presented fewer
operational challenges than disinfecting N95
masks, he stated.
https://www.sciencedaily.com/releases/2020/06/200612172222.htm
UV Sterilization does not Impact Mask Efficiency
According to ASU Studies
Sterilization may alter mask structure and
therefore the effectiveness of the mask’s
ability to block small droplets and aerosols.
Airborne particles and droplets, from a few
nanometers to a few microns in size, are the
research focus of School of Molecular Sciences
Professor Pierre
Herckes.
Herckes and his graduate student researcher,
Zhaobo Zhang, were testing personal protective
equipment (PPE) mask efficiency to trap
nanoparticles in the semiconductor industry
prior to the COVID-19 outbreak. After the
outbreak, they were approached by several groups
to test mask efficiency before and after
sterilization. Sterilization methods included
treatment with ultraviolet (UV) light, ozone, or
peroxide vapors. Before and after each of these
sterilization methods, Herckes and Zhang tested
the efficiency of masks to trap droplets and
aerosols.
“What we found was there was not a significant
decrease in mask efficiency before and after
treatment," Herckes said. "However, further
testing needs to be done to determine the effect
of multiple treatments on the structure of mask
materials.”
Herckes notes that their testing methods differ
from National Institute for Occupational Safety
and Health methods, but nevertheless provide
important results.
Herckes is co-investigator with ASU engineering
professor Paul Westerhoff on a recently funded
National Science Foundation grant, “Disinfection
and Reuse of Health-Care Worker Facial Masks to
Prevent Infection coronavirus disease.” This
grant allows Westerhoff and Herckes to test for
change in mask efficiency after repeated
UV-light exposure.
“This research is important because we know very
little about how UV-light modifies the molecular
structure of protective masks,” Herckes said.
Their work will also allow them to determine
mask efficiency based on particle size and
charge.
Large droplets, such as those produced when
someone coughs or sneezes, are trapped to a
great degree by a mask, and these droplets don’t
travel as far as smaller droplets. Smaller
droplets, however, are also capable of carrying
coronavirus particles. Coronavirus particles are
also transmitted by smaller particles, such as
those produced by talking or breathing. These
small droplets stay in the air much longer than
large droplets, and they are inhaled more deeply
into your lungs.
“Wear a mask, because it not only protects you,
but it protects others,” Herckes said.
Protection from a mask is greatest when it is
worn properly.
“Wearing a mask below your nose allows you to
inhale and exhale droplets, so cover your nose
with the mask, and make sure it fits properly
around your face so there isn’t leakage from the
sides,” he said. If air goes around the mask,
it’s not effectively trapping particles.
Herckes also advises that you minimize touching
your mask once it’s on.
“Your mask should be comfortable and not
restrict air flow significantly," he said. "When
you touch your mask, you are transmitting
contaminants from your hands to your mask, and
from your mask to your hands. More importantly,
the mask will trap airborne virus particles, so
you will be transferring these trapped particles
to your hands, and then from your hands to
whatever you touch, possibly your face, eyes and
mouth.”
Ultraviolet
Sanitization Kit for Masks, Wallets, Keys and
Glasses
Thanks in large part to COVID-19, though clearly
needed long before any international outbreaks,
ultra-violet sanitization kits are finally
coming to market, offering portable pouches that
kill 99.9% of common bacteria, coronaviruses
and, potentially, novel coronavirus,
all within minutes. Phuong Mai, founder and CEO
of P.MAI.,
recently released the travel-friendly Violet
Clean Kit, which
may be the very best way to sanitize your face
mask, phone, keys and more.
The partially collapsible, plug-in bag uses UV-C
light in a fully-reflective interior to sanitize
any small device, gadget or accessory in three
minutes, and is equally as convenient on the go
as it is for daily use in your own home.
Many of the other sanitizers have fewer and less
powerful UV lamps than Violet uses . It uses 12
powerful UV-C lights powered at nearly 10
milliwatts. Their Clean Kit has been
specifically engineered for optimal UV-C light
at germicidal wavelengths. The reflective
interior and magnetic zippers ensure the light
stays in and does not leak, and the convenient
size makes it easily portable. The bag's modern
design is also waterproof and oil-proof. Plus,
you can use the charging cable and dual power
adapter to charge your phone at the same time.
While some products use a 1 amp or 1.5 amp power
adapter, Violet
specifically use a 2A/5V to ensure optimal
output and efficiency.

It is recommended to sanitize phones, keys,
wallet, face mask and sunglasses after being
outside or around people.
North Carolina Meat and Poultry Industry has
Major COVID Problem
The meat and poultry industry in North Carolina
hires over 35,000 workers in the state and can
employ more than 4,000 workers in a single
facility. The state is continuously ranked among
the top five U.S. producers of chickens and
hogs.
But another statistic has emerged in the
industry with grim consequences: Plants that
process meat and poultry also are a breeding
ground for coronavirus. In North Carolina
processing plants, more COVID-19 outbreaks have
occurred than any other state, according to
the Food & Environment Reporting Network (FERN).
When outbreaks occur at densely populated
workplaces like meatpacking plants, it’s not
just the workers who are affected — they can
carry the virus back to their families and
communities. State health data on COVID-19
cases per ZIP code analyzed
by The News & Observer offers a look into the
potential scale of the outbreaks around several
key processing plants.
Coronavirus cases and infection rates per 10,000
residents have risen higher in the zip codes of
counties with significant plant outbreaks — like
Mountaire Farms in Chatham County — compared to
ZIP codes in counties without processing plants.
Across 13 ZIP codes near processing plants with
outbreaks in seven North Carolina counties,
virus cases rose by nearly 600% on average from
May 1 when the data was first released up to
June 11.
In contrast, the number of cases statewide in
the same time frame rose by 262%.
Over 2,000 processing plant workers so far have
tested positive for the coronavirus, according
to state health officials. Not all infected
workers live in the same counties or ZIP codes
they work in, highlighting the potential of
virus spread.
The infection rate per 10,000 residents in these
counties is higher than those of more populous
counties with higher overall cases like Wake,
Durham and Mecklenburg, according to the state’s
daily ZIP code virus data. Here is a
county-by-county look at some of the most
affected areas:
Chatham County
The Mountaire Farms poultry farm in Siler City,
one of the major employers in Chatham County
employing around 1,600 workers, has had
outbreaks since early April. Its ZIP code of
27344 has one of the highest case numbers in
North Carolina with 510 cases as of June 8.
An outbreak is defined by the Centers for
Disease Control as more than two coronavirus
cases.
COVID-19 testing of plant workers and their
families resulted in 74 positive cases among 340
people in late April, The
N&O reported previously,
but the plant
hasn’t reported an updated number of cases
since.
Mountaire is a main employer of many Latinos of
Siler City, who make up 43% of its population,
according to recent census data. Most are
immigrants from Mexico and Central America.
According to Chatham’s newly released ethnicity
COVID-19 data, Latinos are 34% of its positive
cases. But Latinos make up only about 10 percent
of the county’s population.
Robeson County
Three pork and poultry plants with outbreaks —
Mountaire Farms, Sanderson Farms and Prestige
Farms — are located in Robeson County. The
county’s health department told The N&O that by
the end of May, Mountaire had 61 cases, Prestige
had nine and Sanderson had five.
The world’s largest pork processing plant is
Smithfield Foods, which is in adjacent Bladen
County. That plant had 92 cases of workers who
are Robeson residents, the county health
department said.
Several other county health departments told The
N&O previously that some of their residents were
infected through working in that Bladen County
plant. As of June, at least nine residents of
Columbus County, three in Scotland County, three
in Harnett County and one in Johnston County
FERN’s report on plant outbreaks said that pork
plants specifically led in the number of cases
with nearly 6,000 cases as of May 19, followed
by beef and chicken nationwide.
Burke County
The ZIP code of Morganton that contains the Case
Farms poultry plant carries 550 of the entire
county’s 700 cases. Cases shot up after testing
of the poultry workers in early June,
reported The Morganton News Herald.
The plant and the Burke health department has
said they will not release those numbers.
“We are not identifying numbers at any
businesses since these cases are community
spread and it is all over the county,” the
public information officer for Burke County told
The Morganton News Herald this week. “It does
not provide any value to list all the businesses
that have positive cases.”
Case Farms told The N&O previously that they
were contact with the county health department
regarding the outbreak.
Lee County
The Pilgrim’s Pride poultry plant in Sanford has
had an outbreak since early April. Both the
county health department and the plant company
told The N&O they would not disclose case
numbers, though the county organized testing for
the workers.
Cases in the ZIP code of the plant and in an
adjacent ZIP code have tripled since May 1.
Pilgrim’s Pride parent company JBS had the
second-highest cases in its plants across the
nation, according to FERN.
A plant worker who resided in Chatham County died
from COVID-19 complications last
month and also infected his family, The N&O
reported.
Duplin County
The Butterball and Villari Foods plants in
Duplin both have outbreaks. Local TV station
WITN reported in April that Butterball had over
50 cases. Southerly
Magazine reported that
its Latino immigrant workers complained about a
lack of protections there and spread the virus
to their families.
Cases in the zip code of the Butterball plant
tripled to 304 since May 1, but at least 56 of
these cases are attributed to an outbreak at the
two nursing homes, according to NCDHHS.
Wilkes County
Nationally, Tyson Foods has the highest number
of coronavirus cases associated with a poultry
company. They announced that 570 workers tested
positive at its plant
in Wilkesboro last
month, the largest known plant outbreak in the
state. The outbreak shut the plant down
temporarily and infected workers from other
counties — the total cases in the county are
511, less than the plant outbreak.
Coronavirus cases in the two Wilkesboro zip
codes skyrocketed by roughly 1000% since May 1.
Wayne County
Two Wayne County ZIP codes weren’t included in
the average rate of increase because accurate
data before May 20 were not available. Virus
cases in the Neuse Correctional Facility in
Wayne County were being included in two county
zip codes until it was moved to a unique zip
code by NCDHHS.
At least 12 cases in one Wayne ZIP code are from
a nursing home.
Cases have grown in the ZIP codes of Case
Farms’s Wayne County plant — from 12 to 173 —
and also in the town of Goldsboro, a populous
area 20 miles away from the Butterball facility
in Mount Olive, which is split between Wayne and
Duplin counties.
Despite the national outbreaks at these
facilities, the U.S. Department of Agriculture
said in a statement June 9 that meatpacking
facilities are currently operating at over 95%
capacity during the pandemic compared to last
year.
The statement says that Secretary Sonny Perdue
“applauded the safe reopening of critical
infrastructure meatpacking facilities across the
United States.”
Declared a critical industry during the
pandemic, food processing plants have been
ordered to remain open under the Defense
Production Act by a presidential executive
order.
Social Distancing is not a Safe Solution
The conventional wisdom is
that 6
feet of social distance creates a safe buffer,
and restaurants, offices, and
even Starbucks cafes are being redesigned around
that tenet. Social distance does help prevent
transmission, but according to new modeling,
even a small breeze can spread COVID-19 up to 20
feet.
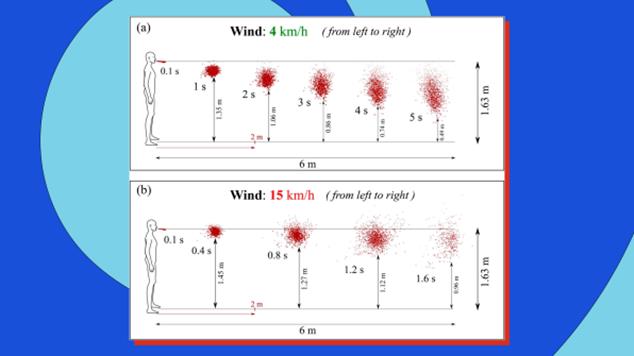 [Image:
Talib Dbouka/Dimitris Drikakis/AIP]
[Image:
Talib Dbouka/Dimitris Drikakis/AIP]
Dimitris Drikakis, the professor at University
of Nicosia, Cyprus, who created the model,
insists that this finding doesn’t mean that
someone coughing 20 feet away will get you
instantly sick. The overall amount of virus you
breathe in overtime matters, too. But his
research does confirm that even outdoors,
distance gatherings come with some risk.
On cruise ships and in many buildings, HVAC
systems use lower-quality air filters, which
might catch just 20% to 40% of viruses passing
through. On the tragic Diamond Princess cruise
ship, which quarantined thousands of passengers
to their rooms for nearly a month while the ship
was dry-docked in Tokyo Bay, air circulated
between cabins without HEPA filtering, infecting
700 people and killing eight people who were
breathing the same old stew of air.
In Fast Company Mark Wilson reports
that
U.S. office buildings may begin to retrofit with
higher-end HVAC systems (with HEPA filters and
even UV light sterilization hiding in the
ducts), which are more common in China, but it’s
hard to quantify how many companies and
landlords are actually taking those steps.
The safest option for quarantining viruses in
the air are negative pressure rooms, which
operate like vacuum cleaners, ensuring that no
pathogens can escape. But they’re designed for
hospitals. They’re not feasible for hotels,
offices, and other buildings for a variety of
reasons—including expense, the difficulty in
validating their design, and the fact that every
office worker in America would need their own
office with a door that is always closed. Only
2% to 4% of all hospital rooms are equipped to
be negative pressure spaces as it is.
Some scientists believe that summer could help
curtail the spread of COVID-19 due to heat.
Indeed, researchers have shown that extreme heat
can kill the virus; Ford even retrofitted police
cruisers to sterilize car cabins with nothing
but the hot air blowing in from the engine.
One component of air quality that hasn’t gotten
as much attention is humidity. Stephanie Taylor,
infection control consultant at Harvard Medical
School, is petitioning alongside companies that
make sensors and humidifiers to improve air
quality, for the CDC and WHO to adopt guidelines
around safe humidity levels—specifically that
indoor humidity should be kept between 40% to
60% (the current recommendation of the EPA).
That’s the range of what most people consider
comfortable humidity indoors, with air that
won’t dry out your nose. (By comparison, the
Mohave Desert ranges from 10% to 30% humidity.)
Taylor’s own interest in humidity began in 2013
when she was studying how infections spread at a
new hospital. Her research isolated just about
every aspect of a hospital you could imagine,
and she discovered a link between infection
rates and humidity in patient rooms. In fact, it
was the single biggest correlation she found. “I
was totally blown away,” Taylor says. “And to
tell you the truth, I was skeptical.”
But Taylor has since validated these findings on
studies at nursing homes and schools. And from
her research and others in the industry, she
identifies three ways that midrange humidity
levels stop the spread of airborne pathogens.
First, when air is too dry, large droplets don’t
fall to the ground as quickly as they normally
would. Instead, they dry out to become smaller
droplets, which float in the air longer (and
also take longer to drop to surfaces, meaning
the surfaces can continue to be contaminated).
Secondly, airborne viruses that thrive in
winter, like coronaviruses, simply aren’t as
infectious when they float through moister
air—whatever tools the viruses use to be
virulent are somehow stunted. “There are a few
theories as to why,” says Taylor. “But to tell
you the truth, I don’t think we fully understand
the mechanism.”
The final reason is that your respiratory immune
system just works better in greater humidity.
Recent research out of Yale exposed mice to a
strain of influenza. The mice were kept in the
same air temperature, but researchers tweaked
the humidity levels. They found that mice in
low-humidity chambers had a worse immune
response. Humidity didn’t actually remove the
influenza droplets from the air; instead, the
air moisture helped their bodies fight off the
virus better—all the way down to the cellular
level in their respiratory system.
Distancing. Filtering. Humidity. None of these
individual solutions can prevent the spread of
COVID-19. But used in combination, we can make
our indoor air safer—to make it through this
pandemic, sure, but also cold and flu season,
and whatever pandemic awaits us in the future.
“This type of infectious disease will come every
few years,” warned Chen, the Purdue
engineer, back in March. “I started doing
research when SARS broke out in 2004. Then
another time was the 2009 influenza from Mexico,
which killed 150,000 people around the globe.
Today we have coronavirus. Every couple of
years, this type of thing will come back.”
Mark Wilson is a senior writer at Fast Company
who has written about design, technology, and
culture for almost 15 years. His work has
appeared at Gizmodo, Kotaku, PopMech, PopSci,
Esquire, American Photo and Lucky Peach.
The full text is shown at
https://www.fastcompany.com/90515931/theres-a-key-way-to-curb-the-spread-of-covid-19-but-no-one-is-talking-about-it
