Coronavirus Technology Solutions
May 21, 2020
A Mask is Not a Mask-Big
Difference in Efficiency and Fit
Hotel Construction Moving Forward
Hotels have a Variety of Safety Measures to Combat COVID
Airborne Virus Particles are Not
Dead Just Dormant
Purchasers of COVID Products at
Hospitals Being Tracked
Hospitals Not Ready For Second
Wave of Virus
Don’t Rely on Vaccines
Air Conditioning in Hot Climates
is Likely to be a Big
Transmission Vehicle
_____________________________________________________________________________
A Mask is Not a Mask-Big
Difference in Efficiency and Fit
An analysis of mask filter media
shows that there are big
differences between materials
and the fit of the mask.
Homemade masks can be
quite efficient on removing
particles such as viruses but
the pressure drop is high. The
fit of the mask means as much as
the media efficiency.
Details of the study are
shown in an ACS publication
https://pubs.acs.org/doi/10.1021/acsnano.0c03252
There is a need to evaluate
filtration efficiencies as a
function of aerosol particulate
sizes in the 10 nm to 10 μm
range, which is particularly
relevant for respiratory virus
transmission. The researchers
carried out these studies for
several common fabrics including
cotton, silk, chiffon, flannel,
various synthetics, and their
combinations. Although the
filtration efficiencies for
various fabrics when a single
layer was used ranged from 5 to
80% and 5 to 95% for particle
sizes of <300 nm and >300 nm,
respectively, the efficiencies
improved when multiple layers
were used and when using a
specific combination of
different fabrics. Filtration
efficiencies of the hybrids
(such as cotton–silk,
cotton–chiffon, cotton–flannel)
was >80% (for particles <300 nm)
and >90% (for particles >300
nm). The researchers
speculate that the
enhanced performance of the
hybrids is likely due to the
combined effect of mechanical
and electrostatic-based
filtration. Cotton, the most
widely used material for cloth
masks performs better at higher
weave densities (i.e.,
thread count) and can make a
significant difference in
filtration efficiencies. Studies
also imply that gaps (as caused
by an improper fit of the mask)
can result in over a 60%
decrease in the filtration
efficiency, implying the need
for future cloth mask design
studies to take into account
issues of “fit” and leakage,
while allowing the exhaled air
to vent efficiently. Overall,
the study
finds that combinations
of various commonly available
fabrics used in cloth masks can
potentially provide significant
protection against the
transmission of aerosol
particles.
Table 1. Filtration Efficiencies
of Various Test Specimens at a
Flow Rate of 1.2 CFM and the
Corresponding Differential
Pressure (ΔP) across the
Specimens
|
flow rate: 1.2 CFM |
|||
|
filter efficiency (%) |
pressure differential |
||
|
sample/fabric |
<300 nm average ± error |
>300 nm average ± error |
ΔP (Pa) |
|
N95 (no gap) |
85 ± 15 |
99.9 ± 0.1 |
2.2 |
|
N95 (with gap) |
34 ± 15 |
12 ± 3 |
2.2 |
|
surgical mask (no gap) |
76 ± 22 |
99.6 ± 0.1 |
2.5 |
|
surgical mask (with gap) |
50 ± 7 |
44 ± 3 |
2.5 |
|
cotton quilt |
96 ± 2 |
96.1 ± 0.3 |
2.7 |
|
quilter’s cotton (80 TPI), 1 layer |
9 ± 13 |
14 ± 1 |
2.2 |
|
quilter’s cotton (80 TPI), 2 layers |
38 ± 11 |
49 ± 3 |
2.5 |
|
flannel |
57 ± 8 |
44 ± 2 |
2.2 |
|
cotton (600 TPI), 1 layer |
79 ± 23 |
98.4 ± 0.2 |
2.5 |
|
cotton (600 TPI), 2 layers |
82 ± 19 |
99.5 ± 0.1 |
2.5 |
|
chiffon, 1 layer |
67 ± 16 |
73 ± 2 |
2.7 |
|
chiffon, 2 layers |
83 ± 9 |
90 ± 1 |
3.0 |
|
natural silk, 1 layer |
54 ± 8 |
56 ± 2 |
2.5 |
|
natural silk, 2 layers |
65 ± 10 |
65 ± 2 |
2.7 |
|
natural silk, 4 layers |
86 ± 5 |
88 ± 1 |
2.7 |
|
hybrid 1: cotton/chiffon |
97 ± 2 |
99.2 ± 0.2 |
3.0 |
|
hybrid 2: cotton/silk (no gap) |
94 ± 2 |
98.5 ± 0.2 |
3.0 |
|
hybrid 2: cotton/silk (gap) |
37 ± 7 |
32 ± 3 |
3.0 |
|
|
|
|
3.0 |
The quilter cotton mask could
have a capture efficiency of
less than 13%. This means that
these masks are not effective in
combatting the virus. Some of
the fabrics which are effective
have a high pressure drop. Most
important the fit of the mask is
a key factor. An N95 mask with a
gap is only 34% efficient on
particles less than 0.3 microns.
The advice about wearing masks
tends to treat all masks as
equal.
In fact there is a world
of difference.
Hotel
Construction Moving Forward
Some of the
world’s leading hotel designers
weighed in on the current state
of the global hospitality
industry, with particular
attention being paid to project
pipelines and the stage of
various hotel developments
around the world. The reaction
to the crisis has been mixed,
with many projects being put on
hold, but others ploughing full
steam ahead.
The stage of
the development obviously has an
impact on whether or not a
project can move forward, as
does the liquidity of the
developer, and developers whose
properties were already funded
are planning on forging ahead,
says Clay
Markham, Vice President,
Global Sector Leader Hospitality
of CallisonRTKL. Darrell
Long, Design Principal
and Regional Managing Director
at Wilson Associates, is
surprised at the number of
developers that are proceeding
with their schemes. “That number
is shockingly large,” he says.
Hotels
have a Variety of Safety
Measures
to Combat COVID
IHG, owner of
hotel chains like
InterContinental and Holiday
Inn, followed many major hotel
companies by announcing new
cleanliness measures on
May 18, in conjunction
with Cleveland Clinic medical
experts and Ecolab and Diversey
hygiene experts. The in-progress
changes may include hotel-wide
extra deep-cleaning of
high-touch surfaces, "last
cleaned" charts and social
distancing practices. Other
changes might be individual
amenity cleaning kits for
guests, plus hand sanitizer and
disinfecting wipes in guest
rooms.
Four Seasons is
partnering with Johns Hopkins
Medicine International for its
new global health and safety
program, "Lead With Care." The
program notes that public areas
will be cleaned hourly, with
extra attention to areas like
the front desk counters and
public restrooms; kits with
masks, hand sanitizer and
sanitization wipes will be in
each guest room; and restaurants
and bars might operate at a
limited capacity for social
distancing purposes, among other
initiative
Omni's "Safe & Clean" initiative includes
a daily health screening for
employees, with a temperature
check. The company is expanding
its use of Environmental
Protection Agency- and Centers
for Disease Control and
Prevention-approved
disinfectants. Omni is
increasing the cleaning of its
heating and cooling systems and
replacing air filters more
often. High-traffic areas will
become one-way where possible.
Single-use items will be placed
in guest rooms, and a
limited-contact check-in and
check-out process will become
standard.
Caesars Entertainment is
assuring guests its employees
are well-versed in cleaning and
disinfectant practices, which
includes PPE use. Multiple
handwashing stations have been
added to the resort, and both
slot machine banks and table
games will allow for social
distancing going forward, among
other changes.
MGM
launched its "Seven-Point Safety
Plan," a new standard created
with medical and scientific
experts to curb the spread of
coronavirus, respond to possible
new cases and keep customers and
employees safe.
In addition to upgraded incident
response protocols and
contactless check-in, some of
the company's focuses will be:
-
Screening,
temperature
checks and
employee
training:
Employees will
be screened for
signs and
symptoms of
infection and
will continue to
go through
temperature
checks. Guests
are encouraged
to adhere to CDC
guidelines for
self-quarantine
and to not
travel if they
think they have
been exposed.
-
Mandatory masks
and PPE:
Employees will
be given an
approved mask to
wear when on the
property, and
guests are
encouraged to
wear masks in
public areas.
Free masks will
be offered to
guests who need
one. Guests
should limit the
amount of time
they are
drinking on the
casino floor and
should not eat
there.
-
Physical
distancing:
Floor guides
will be
throughout
properties
making sure
people adhere to
six-foot
distancing. But
MGM is aware
distancing could
prove difficult.
"From
time-to-time,
six-foot
distancing will
be challenging –
and in those
cases,
reasonable
mitigating
protocols will
be implemented,
such as
plexiglass
barriers or eye
protection for
employees,"
according to the
new policy.
-
Hand washing and
enhanced
sanitization: On
top of enhanced
cleaning, MGM
will deploy
electrostatic
sprayers for
more efficient
disinfecting.
Hand washing and
sanitizing
stations will
also be
available in
high-traffic
spots, along
with signage.
-
HVAC controls
and air quality:
MGM has worked
to minimize risk
of virus
transmission
with HVAC
systems. HVAC
systems will be
reviewed and
adjusted pending
science and
government
guidance.
Wyndham,
which has more than 6,000 hotels
in the U.S., announced a new
initiative called "Count on Us",
which includes updated cleaning
and disinfection procedures for
guest rooms and public spaces,
plus easy access to health
essentials.
The chain will ship products
including face masks for hotel
employees, disinfectant wipes
for guests and hand sanitizer.
Wyndham is also set to partner
with Ecolab to use its
disinfectants across guest rooms
and public spaces.
Sandals and Beaches Resorts,
which has 24 properties in seven
countries, has its own new
sanitation rules. The chain's
Platinum Protocols of
Cleanliness Program will
include precautionary
temperature checks, personal
anti-bacterial hand towels and
individual in-room hand
sanitizer, according to Sandals
spokesperson Rachael Salzer.
Each hotel room will be
maintained using UV-LED lighting
equipment to inspect
cleanliness, air duct
sanitization for each arrival
and upon each departure and
weekly carpet steam-cleaning.
Hilton is
partnering with the company
behind Lysol, as well as
the Mayo Clinic, to better
ensure cleanliness in its
hotels. The new program will be
called "Hilton CleanStay" and
aims to give guests peace of
mind when staying at a Hilton
property, whether they are in
guest rooms, restaurants, the
gym or other public areas.
Full details are being ironed
out, but several initiatives in
development include:
-
An official room
seal indicating
that a room
hasn't been
accessed after a
deep cleaning
-
The removal of
pen, paper and
guest
directories in
favor of a
digital option
(or available on
request)
-
Contactless
check-in, where
guests can
complete
check-in and
check-out
processes via a
mobile app and
receive a
digital room key
(Hilton Honors
members already
have access to
digital keys)
-
Electrostatic
sprayers and
ultraviolet
light to be used
in the
sanitization
process
Marriott said
it will use electrostatic
sprayers with hospital-grade
disinfectants to sanitize
throughout its hotels. In
addition to guest rooms, the
sprayers will be used in
lobbies, gyms and other public
areas. It said the cleaning
agents used would be those
recommended by the CDC and
Prevention and the WHO to kill
all known pathogens.
In addition, the company is
testing ultraviolet light
technology for sanitizing room
keys and adding hand sanitizer
stations and signs in the lobby
to remind anyone who enters to
keep their distance from others.
Marriott is also taking a look
at what to do at properties that
offer buffet service.
Airborne Virus Particles are Not
Dead Just Dormant
Scientists previously thought
that the viral droplets
traveling some distance were
dead, but new research shows
that they are simply dormant and
waiting for a new source of
rehydration.
In fact, Stephanie Taylor, a
Harvard Medical School lecturer,
studied the effect of hospital
environments on human health and
found that when air is dry,
"droplets and skin flakes
carrying viruses and bacteria
are launched into the air,
travelling far and over long
periods of time. The microbes
that survive this launching tend
to be the ones that cause
healthcare-associated
infections." It turns out that
humans are an ideal source of
hydration - made up of 60%
water. Compounding exposure, dry
air also interferes with our
natural immune barriers, humid
in nature, which makes us even
more susceptible to infection.
While the NIH is still studying
the issue, other studies seem to
confirm her findings. A team at
the Mayo Clinic humidified half
of the classrooms in a preschool
and left the other half alone
over three months during the
winter. Influenza-related
absenteeism in the humidified
classrooms was two-thirds lower
than in the standard classrooms.
Further, many older hospitals,
especially those found in urban
areas, lack effective
ventilation systems or
negative-pressure patient rooms
that can filter out airborne
contaminants. Many built before
the 1950s, these older hospitals
have simply not made the type of
upgrades to their systems over
time that would mitigate the
amount of contaminated air
circulating on the inside of a
hospital.
Purchasers of COVID Products at
Hospitals Being Tracked
Coronavirus Technology Solutions
is including contact information
for those interested in COVID
mitigation in specific end user
groups. Presently contacts at
meat processing plants and
healthcare architecture and
planning firms have been posted.
The next group will be those at
the 100 top hospitals in the
U.S. Note that the top 20
hospitals have more than1000
beds each
1. New York-Presbyterian
Hospital/Weill Cornell Medical
Center (New York City) – 2,2591
2. Florida Hospital Orlando –
2,2422
3. Jackson Memorial Hospital
(Miami) – 1,7323
4. Methodist Hospital (San
Antonio) – 1,5854
5. UPMC Presbyterian
(Pittsburgh) – 1,5835
6. Yale-New Haven (Conn.)
Hospital– 1,5526
7. Orlando (Fla.) Regional
Medical Center– 1,5107
8. Montefiore Hospital-Moses
Campus (Bronx, N.Y.) – 1,4388
9. Baptist Medical Center (San
Antonio) – 1,4229
10. Indiana University Health
Methodist Hospital
(Indianapolis) – 1,37210
11. Methodist University
Hospital (Memphis, Tenn.) –
1,36711
12. Barnes-Jewish Hospital (St.
Louis) – 1,335
13. Norton Hospital (Louisville,
Ky.) – 1,29512
14. The Cleveland Clinic – 1,277
15. The Mount Sinai Medical
Center (New York City) – 1,22113
16. Memorial Hermann Southwest
Hospital (Houston) – 1,17614
17. Buffalo (N.Y.) General
Hospital – 1,15915
18. UAB Hospital (Birmingham,
Ala.) – 1,118
19. North Shore University
Hospital (Manhasset, N.Y.) –
1,07616
20. Beaumont Hospital, Royal Oak
(Mich.) – 1,070
https://www.beckershospitalreview.com/lists/8-7-14-100-largest-hospitals-in-america.html
Hospitals Not Ready For Second
Wave of Virus
Hospitals will not be ready for
a renewed onslaught of
coronavirus infections if a
second wave comes in the fall, a
Rhode Island emergency physician
told Congress on Thursday, May
21.
“I do not think that we are
currently prepared for a second
wave,” Dr. Megan Ranney,
emergency physician and
Associate Professor of Emergency
Medicine at Brown University,
testified before the House
Select Subcommittee on the
Coronavirus Crisis.
Several medical experts,
including US Centers for Disease
Control and Prevention director
Dr. Robert Redfield, have
predicted coronavirus
could start spreading fast again
in the autumn,
and said it would be complicated
by the beginning of a fresh
influenza season, too.
There has not been enough
preparation for that, Ranney
told the hearing.
“We still lack adequate
protective equipment in most
hospitals across the country,” Ranney
said. “On a national level, we
still are millions and millions
and millions of pieces of PPE
short from what hospitals need
currently; much less what they
need in order to build the
normal stockpiles that we all
keep in order to face pandemic
situations.”
Staff are having to reuse
equipment meant to be thrown out
after every patient encounter –
a dangerous practice. “We would
never have reused an N95s for an
entire shift. We never would
have reused surgical masks in
between patients and that's what
we're doing now,” Ranney said.
Plus, more research is needed,
she said. “We also still lack
adequate science,” Ranney
said. “I'm so thankful for the
funding that you all have given
to NIH and CDC but it's not
enough, and we need more.”
But most of all, Ranney
said, the US needs “adequate
testing for frontline workers,
not just in healthcare, not just
in nursing homes and sniffs and
hospitals, but also all of you
who have testified today.”
Don’t Rely on Vaccines
The global case tally for the
coronavirus that causes COVID-19
passed 5 million on Thursday
after the biggest one-day
increase since the start of the
outbreak, as a top U.S.
scientist cautioned that people
should not rely on a vaccine and
the labor market continued to
show massive job losses.
William Haseltine, a scientist,
biotech entrepreneur, and
infectious disease expert, is
chair and president of the
global health think tank ACCESS
Health International and said
the best way to manage the
pandemic is through measures
such as isolation, testing and
contact tracing and observing
social-distancing, face masks
and frequent hand washing.
“Do not listen to the
politicians who say we’re going
to have one by the time my
reelection comes around,” he
said. “Maybe we will (but) I’m
just saying it’s not a slam-dunk
case by any means ... because
every time people have tried to
make a vaccine – for SARS or
MERS – it hasn’t actually
protected.”
His comments came as the
director of the Centers for
Disease Control and Prevention
warned that the virus is likely
to return in the fall and winter
and may force a fresh round of
lockdown measures. Robert
Redfield told
the Financial Times that
the U.S. needs to speed up its
disease-tracking capabilities in
the next few months to avoid
another public health crisis.
“We’ve seen evidence that the
concerns it would go south in
the Southern Hemisphere like flu
[are coming true], and you’re
seeing what’s happening in
Brazil now,” Dr. Redfield told
the FT. “And then when the
Southern Hemisphere is over, I
suspect it will reground itself
in the north.”
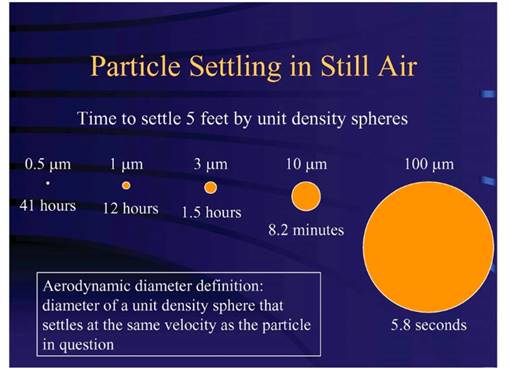
Air Conditioning in Hot Climates
is Likely to be a Big
Transmission Vehicle
The Federation of European
Heating, Ventilation and Air
Conditioning Associations
(REHVA) in Europe had warned
that the coronavirus could stay
airborne for some time and
travel long distances. Architect
Justin Bere noted that "It
recommends avoiding central
recirculation during SARS CoV-2
episodes and closing the
recirculation dampers, even if
there are return air filters. As
the REHVA guidance says, these
don’t normally filter out
viruses." Bere explained:
Recent research indicates that
large droplets from sneezing can
travel much further than 2
meters, even if there are no air
movements. Small particles (<5
microns), generated by coughing
and sneezing, may stay airborne
for hours according to the REHVA
guidance and can travel long
distances. A Coronavirus
particle is only 0.8 to 0.16
microns diameter so there could
be many virus particles in a
5-micron droplet floating around
in the air.
They have been studying the
problem in Canada too. Professor
Brian Fleck told
the National Post that
"this has been on people’s radar
for quite a while,” he said.
“Somebody on a different floor
sneezes …The particle can stay
airborne long enough to go all
the way through the system and
then pop out in somebody else’s
office.
There are various ways that the
risk can be lessened, including
use of filters that catch a
greater number of those
particles, and drawing more
fresh air into a system....But
each of those changes carries a
cost. Adding more fresh air can
require additional heat or air
conditioning. Heavier filters
means more energy is needed to
push the air through them.
But
it doesn't get as hot in Canada
as it does in Arizona. Engineer
and Professor Ted Kesik told
TreeHugger that "we shall be
greatly challenged retrofitting
our existing buildings to
eliminate dilution ventilation
systems." This is especially a
challenge in the heat of a
southern summer, where the
difference between inside and
outside air can be 40°F in
Arizona or Texas. In the
Southeast, there is also a lot
of humidity with the heat.
That's why the air is
recirculated; the amount of
energy needed condition a mall's
worth of outside air would be
ridiculously high.