
Coronavirus
Technology Solutions
February 24, 2021
Over 25 Million
Masks will be
Distributed to
Underserved
Communities
Singapore
Residents
Receiving Free
Masks
Follow the
Taiwan Example
and Supply Free
Effective Masks
to Everyone at
Princeton
Local Groups
Providing Masks
for the
Vulnerable
OSHA Should Set
Air Standards in
Work Places
Americans will
Still be Wearing
Masks in 2022
Need to Focus on
Length of Mask
Use
GW University
Creating HVAC
Systems Which
Minimize
Horizontal Air
Flow
_____________________________________________________________________________
Over 25 Million
Masks will be
Distributed to
Underserved
Communities
The Biden
administration
announced
Wednesday
it would
distribute more
than 25 million
masks to over
1,300 community
health centers
and 60,000 food
pantries and
soup kitchens in
an effort to
reach
underserved
communities and
as part of the
president's
promise to make
the pandemic
response more
equitable.
Between March
and May, the
administration
will send
well-fitting cloth
masks, available
in child and
adult sizes,
that can be
washed for
reuse, White
House COVID-19
response
coordinator Jeff
Zients announced
during a press
briefing.
The masks will
also be
compliant with
coronavirus
guidance from
the Centers for
Disease Control
and Prevention,
made in the U.S.
and will not
affect the
availability of
masks for health
care workers.
"Not all
Americans are
wearing masks
regularly,
not all
Americans have
access and not
all masks are
equal," Zients
said. "With this
action, we are
helping to level
the playing
field, giving
vulnerable
populations
quality,
well-fitted
masks."
The Department
of Health and
Human Services,
in partnership
with the
Department of
Defense, will
deliver masks to
Federally
Qualified Health
Centers. Among
these health
centers,
two-thirds of
the people
served live in
poverty, 60% are
racial or ethnic
minorities, and
nearly
1.5 million
are homeless,
according to a
fact sheet
provided by the
White House.
The Defense
Department will
work with the
Department of
Agriculture to
deliver masks to
about 300 food
banks that
extend across a
network
of 60,000 food
pantries, soup
kitchens and
other food
distribution
points.
Americans can
pick up
individual
wrapped masks at
any of these
locations,
Zients said.
About 12 million
to 15 million
Americans are
expected to
receive masks as
a result of this
campaign, the
White House
said.
The campaign
rollout came a
day after Biden
told essential
workers at a
virtual
roundtable that
he expected his
administration
to send millions
of masks around
the country
"very shortly."
Studies have
shown, and Dr.
Anthony Fauci
has pointed out
many times,
masks are the
single most
effective way to
protect yourself
and others from
getting infected
with the
coronavirus that
causes Covid-19.
"Masks are a
two-way street.
Masks protect
you and me" by
preventing the
spread of
droplets and
aerosol that may
contain the
virus, the US
Centers for
Disease Control
and Prevention
says in its mask
guidance.
Biden has called
on everyone to
wear a mask when
out in public,
and he has made
it mandatory on
federal
property. Masks
are required on
public
transportation
and in airports
and transit
stations.
Most states and
some local
governments have
some type of
mask mandate in
place, and most
retailers
require shoppers
to wear them in
their stores.
Earlier this
month, White
House chief of
staff Ron Klain
said that the
Biden
administration
is hoping to
resurrect a
proposal from
the Trump
administration
to send masks
directly to
Americans.
"This was an
idea that really
came up last
year in the
Trump
administration
-- the public
health agencies
recommended it,
President Trump
vetoed it for
some reason,"
Klain told NBC's
Lester Holt on
February 4. "We
want to get this
back on track. I
hope in the next
few days, or
next week, we
may be able to
announce some
progress on
this."
The US Postal
Service had
planned to
distribute 650
million face
coverings for
the Trump
administration
last April,
according to
internal
documents reviewed
by CNN in
September.
A senior
administration
official told The
Washington Post at
the time that
the plan was
scrapped by the
White House as
some advisers
were worried
that it could
create "concern
or panic."
"If you're
wearing a cloth
mask, it should
be a
multi-layered
mask so that you
have several
layers of
potential
protection for a
single mask,"
CDC Director Dr.
Rochelle
Walensky
recently told
CNN's Anderson
Cooper and
Sanjay Gupta.
The CDC has
recently updated
its guidance to
suggest wearing
a cloth mask
over a
disposable mask,
such as one of
those blue
surgical masks,
as a way to add
more protection.
New data from
the CDC shows
that layering a
cloth mask over
a disposable
medical mask can
block 92.5% of
potentially
infectious
particles from
escaping by
creating a
tighter fit and
eliminating
leakage.
Fauci, director
of the National
Institute of
Allergy and
Infectious
diseases, has
recently sported
two masks, one
on top of the
other.
The original
program involved
cloth masks made
by underwear
manufacturers.
As you
can see from the
draft USPS News
Release below
there would have
been five masks
per household.
These
were washable
masks. So a use
period of a week
or two was
likely
envisioned.
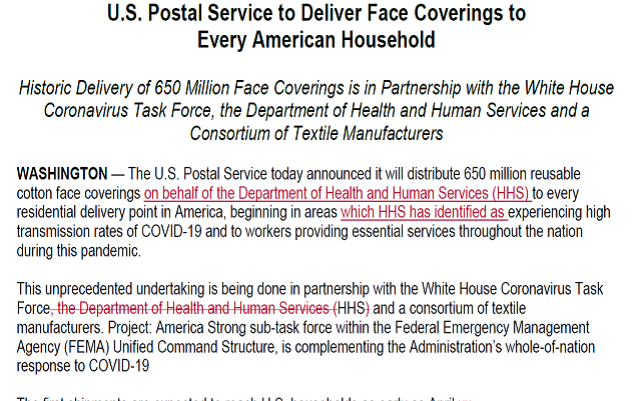
The consortium
of Textile
Manufacturers at
the time
included Hanes
“HanesBrands is
part of a
consortium of
apparel
manufacturers
that have a
contract with
the U.S. federal
government to
produce cotton
masks.
HanesBrands aims
to produce 1.5
million of these
masks weekly,
with the entire
consortium to produce
5 million to 6
million each
week, using
HanesBrands’
design and
patterns as the
guide.”
Singapore
Residents
Receiving Free
Masks
Residents in
Singapore will
be able to
collect free
reusable masks
and alcohol-free
hand sanitizer
from March and
April, in
another
nationwide distribution
by Temasek
Foundation.
In a Facebook
post, Temasek
Holdings CEO Ho
Ching said the
reusable masks
will be ready
for collection
on Mar 1. Every
Singapore
resident can
each collect one
navy-blue mask
from Swiss
company
Livinguard,
provided by
the
Temasek
Foundation, she
said in the post
last Friday (Feb
19).
"Like before, we
cover
Singaporean and
non-Singaporean
residents, as no
one is safe till
everyone is
safe," said Mdm
Ho.
This is the
fourth national
mask
distribution by
Temasek
Foundation, and
the collection
will last for
two weeks.
Between June
last year and
end-January,
about 26 million
reusable masks
have been
distributed,
Temasek said in
a Facebook post
on Jan 28.
The new
mask is made up
of two layers -
the outer layer
is a water
repellent
antimicrobial
layer while the
antibacterial treatment
on the inner
layer "kills any
bacteria from
our saliva",
said Mdm Ho.
The mask also
does not have to
be washed after
daily use, she
said. Instead,
the mask can be
washed once or
twice a week.
With up to 30
washes, the
mask can be used
daily for about
six to seven
months.
Even after 30
washes, the mask
can be used as
an ordinary
two-layer cotton
mask. It can
also be used as
an "outer mask"
to provide
better
protection for
those who may be
wearing another
mask
underneath.
"For instance,
if there should
be an outbreak
of the more
infectious
variants from
UK, South Africa
or Brazil, we
should use a
double mask for
extra
protection,"
said Mdm Ho.
Follow the
Taiwan Example
and Supply Free
Effective Masks
to Everyone at
Princeton
Mark Lee, a
graduate student
in the School of
Public
and
International
Affairs at
Princeton has
written an
insightful
article which
champions a
program
to
provide free
effective masks
to not only
those directly
associated with
the University
but also the
towns people.
It is in
a large part
what McIlvaine
is proposing
with safe
bubbles.
(McIlvaine was a
graduate of this
same school
decades ago).
Here are
excerpts from
Mark’s article.
“On Jan. 31,
Taiwan announced a
$7 million
initiative to
secure surgical
masks for its
entire
population of 22
million. In a
massive
public-private
partnership, the
government
devised a
five-week plan
to produce more
than 10 million
masks per day
and meet the
nation’s rising
demand for
protection,
managing mass
distribution
through a newly
developed online
platform.
It is a
remarkable
story,
especially when
you consider the
announcement was
made more than a
year ago, on
Jan. 31, 2020.
(And in case
you’re
wondering, the
initial
production
target was achieved ahead
of schedule.)
By early spring
2020, Taiwan’s
neighbors were
also assembling supply
chains
and implementing innovative
technologies to
get quality
masks in the
hands of
citizens. With
3M’s patented
N95 mask —
the gold
standard of face
masks — facing
worldwide
shortages, some
East Asian
countries began
mass-producing
their own
alternative
versions that 3M
itself acknowledges are
“similar” in
filter quality.
Still reeling
from tragedy in
Wuhan, China
boosted its mask
production
capacity by 450
percent in one
month. After
overcoming
early quality
concerns, China
now
widely exports its
own KN95 masks
for medical use
around the
world.
Meanwhile, South
Korea launched
a national
initiative to
distribute its
KF94 masks at an
accessible price
of $1.20 per
mask. Despite
some initial
hiccups,
officials in
these countries
took the
measures
necessary to
protect their
citizens,
including
communicating
the reasons why
everyone should
wear and have
access to
high-quality
masks.
Meanwhile, the
U.S. government
lagged far
behind. On Feb.
29, the U.S.
Surgeon General
was
still tweeting that
face masks were
"NOT effective,”
and by the time
the Centers for
Disease Control
and Protection
(CDC) finally
recommended face
coverings on
April 2, it was
far too late.
During New
York’s first
wave,
medical-grade
masks (i.e.,
anything with at
least the
protective
quality of a
surgical mask)
were in
disastrously short
supply.
Americans were
forced to
fabricate their
own protection,
with the U.S.
Surgeon General
publishing
a video on how
to make a mask
out of an old
t-shirt. For
several weeks,
even front-line
health workers
were furnishing
their
own homemade coverings.
In the months
since, multiple
North American
and European
researchers
have published new
studies
“proving”
what health
leaders in East
Asia already
knew when they
began taking
action over one
year ago:
quality masks
matter, and it's
effective public
policy to ensure
affordable
access and
widespread
adherence during
a pandemic.
Despite this
scientific
truth, it was
only this week
that the U.S.
government
finally encouraged widespread
adoption of
medical-grade
masks, based on
a new CDC
study demonstrating that
their use could
help limit the
spread of the
virus. Yet
this report did
not come with an
accompanying
plan to
guarantee
affordable
access for all.
In lieu of a
nationwide or
statewide mask
distribution
scheme,
Princeton would
do well to
proactively
launch its own
in our
community. This
semester, the
University has
the opportunity
to follow the
example of
Taiwan and
embark on a
similar project,
though on a much
smaller scale.
By procuring and
distributing
medical-grade
masks to all
members of the
Princeton
community — both
on campus and in
town — the
University can
take a simple,
evidence-backed
measure that
will keep our
community safer
as we continue
to weather this
devastating
pandemic.
As a master’s
student at the
School of Public
and
International
Affairs and a
Resident
Graduate
Student, I have
had the immense
privilege of
remaining in
student housing
ever since our
initial lockdown
last March. I
have watched
firsthand as
Princeton has
leveraged its
wealth to
operate almost
like an
independent,
well-resourced
nation,
imitating public
policy decisions
successfully
applied in
Taiwan, South
Korea, New
Zealand, and
elsewhere.
Indeed, the one
notable area
where Princeton
has yet to take
substantive
action is
quality mask
access, even
though
medical-grade
masks (other
than N95s) are no
longer in short
supply.
Since August,
the University
has paid for
weekly
asymptomatic
testing for all
students, staff,
and faculty. As
Taiwan pioneered in
early 2020, the
University
mandates
quarantine for
incoming
travelers, and,
crucially,
provides free
meals as well as
grocery delivery
for graduate
students living
in apartments.
Although I never
tested positive
for COVID-19,
the moment I
reported mild
symptoms in
December,
University
Health Services
stepped in to
provide care,
calling me daily
for wellness
checks while I
isolated in my
dorm room as a
precaution. I
feel extremely
privileged to
have access to
this safety net,
which includes
resources far
beyond the reach
of the average
American, never
mind the
millions of
essential
workers who are largely Black
and Brown.
I also feel
grateful to live
in New Jersey,
where more than
90 percent of
residents are complying with
mask wearing.
I’m especially
appreciative of
University
employees for
abiding by these
measures,
including campus
dining cooks
working over hot
stoves and other
facilities staff
engaged in
physical labor.
Unlike other
parts of the
country, we
aren’t dealing
with mask
deniers or
questionable
mask adherence.
It’s clear that
members of our
community listen
to public health
officials and follow
guidelines and
would readily
adopt
medical-grade
masks if
provided access
and clear
instruction.
That’s why it
alarms me to see
dozens of
students and
staff still
wearing flimsy
cloth masks,
bandanas, or
gaiters as face
coverings on
campus, despite mounting
evidence that
these makeshift
options do not
offer adequate
protection. On
Feb. 10, the
CDC announced new
research that
COVID-19
transmission can
be reduced by up
to 96.5 percent.
If individuals
wear
“well-fitting”
masks with
multiple layers
that can be
adjusted to the
user’s face,
design features
that are
incorporated
into both Korean
KF94 and Chinese
KN95 masks.
Higher-quality
masks are more
critical than
ever given the
emergence of
more infectious
variants, as recently
flagged by
medical experts.
Fortunately, the
cost to provide
better masks
would be a drop
in the bucket
compared to the
significant
expenses the
University has
already
dedicated to
ensuring safety
on campus, which
have included establishing our
own campus
testing
laboratory and
administering
twice-weekly
coronavirus
tests for
students.
Although the CDC
still limits the
use of N95s to
health
personnel, KF94
and KN95 masks
are available for
purchase
for under two
dollars each,
for a total cost
of less than $10
per student per
week. It would
be a worthwhile
and affordable
investment for
Princeton to
acquire these
masks in bulk,
distribute them
to everyone on
campus, and
educate all on
why they are a
better choice
than less
protective
coverings.
Simultaneously,
these
high-quality
masks must also
be made
available to
members of the
nearby
community.
Whether at the
grocery store or
downtown
businesses,
local residents
come into
contact with
Princeton
students on a
daily basis.
Even registered
family members
of students
living in
graduate housing
face barriers
accessing the
University's
medical
resources; I
have several
classmates whose
partners are
excluded from
asymptomatic
testing and
aren’t able to
access referrals
to specialists
on the MyUHS
website, despite
being officially
registered with
the University
as cohabitating
spouses.
As local organizers
are highlighting
at
a demonstration this
weekend, we have
to acknowledge that,
especially in a
pandemic, we are
one Princeton
community, and
our collective
safety and sense
of community
care does not
diminish the
moment we cross
Nassau Street
into town.
During a year of
chaos and
uncertainty,
Princeton has
utilized its
vast resources
to take decisive
action and
successfully
secure our
campus. As we
adapt to the
next phase of
this pandemic,
it’s time for
our health
leaders to
procure better
masks and once
again keep our
community safe.”
Mark Lee is
Master of Public
Affairs
candidate at the
Princeton School
of Public and
International
Affairs from
Irvine, Calif.
He can be
reached at
markml@princeton.edu.
Local Groups
Providing Masks
for the
Vulnerable
A new program
launched by the
United Way of
Thunder Bay,
Canada
is
providing free
face masks to
those in need
during the
COVID-19
pandemic.
Facing Forward
is a
collaboration
between the
United Way, City
of Thunder Bay,
Thunder Bay
Community
Foundation and
Thunder Bay
District Health
Unit.
"Vulnerable
community
members who
might not
otherwise be
able to afford
to buy a mask
will have access
to free a mask,"
said United Way
of Thunder Bay
CEO Albert
Brule. "And
there's a
combination of
disposable
masks, which are
best suited to
certain
situations, and
reusable cloth
now that we are
making available
to those who
can't afford to
buy them."
The program
offers a few
ways for people
to get involved.
Those buying an
individual mask
at Ungalli
Clothing Co. on
Cumberland
Street S. will
also provide one
free mask to a
vulnerable
community
member.
Businesses can
buy masks in
bulk online,
with proceeds
supporting the
Facing Forward
program.
OSHA Should Set
Air Standards in
Work Places
Dr. David
Michaels led the
Occupational
Safety and
Health
Administration,
which sets
workplace
standards,
during the Obama
administration.
Now the
epidemiologist
is one of more
than a dozen
scientists
calling on the
Biden
administration to
set air
standards for
workplaces like
grocery stores,
meatpacking
plants, buses
and prisons, to
save lives in a
pandemic.
We’ve known for
nearly a year
that COVID is
airborne – yet
aside from
hospitals, few
workplaces
acknowledge that
the virus can
hang in the air,
he told Julie
O’Connor of the
Star-Ledger
Editorial Board.
Instead, they
emphasize
surface-scrubbing
and physical
distancing.
Below is an
edited
transcript.
Q. So the
federal Centers
for Disease
Control has set
no standard for
ventilation? Not
even for
schools?
A. That’s right.
There are
private groups
that put out
voluntary
standards, but
there are no
actual standards
for ventilation
right now.
Q. We’ve
followed the
debates over
ventilation in
school
buildings. Can
you talk about
how this is
playing out in
other
workplaces, if
at all?
A. The debate is
not so much
about schools or
specific
workplaces, but
how COVID-19 is
transmitted.
Early in the
pandemic, we
very much
focused on
larger droplets
and contaminated
surfaces. We
now understand
that breathing
tiny particles
called aerosols
also spread the
virus. And
because of that,
we need to
implement other
sorts of
precautions.
Simply keeping
people six feet
away and
cleaning
surfaces and
wearing a
surgical mask or
a cloth mask is
not adequate.
Q. Those are the
kinds of things
Gov. Murphy has
directed
employers to do.
You’re arguing
it’s not enough
to keep workers
safe.
A. Exactly.
They’re
important. But
distancing is
not always
adequate; we
know that people
who are exposed
at distances far
greater than six
feet have gotten
sick. If
you can make
sure the virus
is not in the
air, that’s the
best.
One part of it
is to make sure
people who are
sick stay home.
But we want to
dilute the
workplace with
fresh air or
filtered air as
much as
possible. And
surgical masks,
while useful in
keeping droplets
out of the air,
are less
effective in
controlling
aerosols. In
some situations,
for heavily
exposed workers
in risky
environments for
longer periods,
we probably need
stronger masks,
like
respirators.
Q. You think the
government
should be
setting air
standards for
workplaces and
requiring N95s
or other
respirators?
A. Yes. What
we’re asking the
CDC to do is
recognize this
means of
transmission is
an important one
and modify its
guidance to
reflect this.
That will be
important
because OSHA is
likely to be
issuing an
emergency
temporary
standard for
workplaces
within the
month. It will
point to CDC
guidelines and
say, follow
this. And if the
guidelines are
out of date,
they will be
less protective.
Q. What might
this mean for
workers?
A. In the most
hazardous
workplaces like
meat or poultry
factories, many
employers have
left people
working shoulder
to shoulder and
put pieces of
plastic film
between them.
The idea is that
if you have
workers
breathing or
coughing
droplets, the
plastic will
stop that from
getting into the
breathing zone
of other
workers. We know
that’s not
effective. And
we know there
are studies
where workers
who are at a
great distance
from sick
workers do get
infected.
So what would
have to happen
is, the employer
first would look
to improve the
fresh air flow,
to bring more
outside air, and
use a higher
efficiency
filter to catch
these aerosols.
And if that
weren’t
effective
enough, the
workers who are
there all day
long perhaps
would have to
wear
respirators, as
industrial
workers in many
situations
unfortunately
have to do. I
don’t say N95s,
because there
are more
comfortable
respirators to
use outside of
hospitals, and
there is no
shortage of
them.
Q. Right now,
the CDC is
recommending
double-masking.
A. We’re not
saying that’s
wrong at all.
And we’re not
saying the
public should be
wearing N95s. On
a bus, for
instance, the
riders come in
and out and
don’t need extra
protection. They
could wear a
double mask. But
the bus driver,
or the hospital
worker who’s not
directly working
with COVID
patients but is
nearby – those
workers are in
an environment
where there’s
lots of virus in
the air. Those
people should be
the focus of
better
protection.
Q. I could see
requiring buses
to open windows.
But what might
this mean in a
jail or food
processing
plant?
A. It isn’t
one-size-fits-all.
An employer
could be
required to do a
risk assessment
and make a plan.
The approach
could be to have
fewer people in
the room. It
could be
increasing the
airflow. But
simply saying
distancing and
handwashing and
surface washing
is not adequate.
Q. In the Trump
administration,
you say, OSHA
was pretty
hands-off.
A. Yes. OSHA
received
thousands of
complaints, made
very few
in-person
inspections and
when it did, issued
generally pretty
low fines.
In the meat
packing plants,
hundreds of
workers were
sickened and
some died. And
the fines were
in the $15,000
range. It’s
worth noting
that the place
where the
largest number
of inspections
occurred, and
citations were
issued for
COVID, was the
NY/NJ area. I
think they may
have done as
many inspections
as the rest of
the county
combined. That
was because the
regional
leadership of
OSHA had some
very creative
dedicated,
sophisticated
leadership.
Q. We had a lot
of deaths in
nursing homes.
That could be
another reason.
A. A higher
death rate than
any other state. They
certainly went
to nursing homes
because that was
the problem. But
other parts of
OSHA didn’t do
inspections in
the same way, or
the same numbers
as this region.
It wasn’t
because it was
the worst
problem. Every
state has
nursing homes
that were
disasters.
Q. What are
other most
dangerous
workplaces,
aside from those
you’ve
mentioned?
A. Grocery
stores, which
are open all the
time. Migrant
farm workers.
Many are brought
to the fields in
vans provided by
their employer,
where they are
exposed to each
other, and live
in bunk houses.
You can’t wear a
mask and you
have sometimes
poor
ventilation.
Q. The CDC has
not recommended
N95 masks or
other
respirators,
even with the
emergence of the
more contagious
variants and
slow vaccine
rollout. Are
they worried
consumer use
would fuel
another
shortage?
A. We no longer
have a shortage
of N95s, and
there are other
respirators
available that
wouldn’t compete
with health care
for use.
Q. Do you think
the Biden
administration
is likely to
require industry
to invest in
better masks and
ventilation?
A. I think there
will be
requirements for
better
protection for
workers.
Q. What would
you say to a
struggling
restaurant owner
who says, ‘I
can’t afford to
buy everybody
these masks or
fix the
ventilation’?
A. I think we’re
going to need to
subsidize small
businesses to
keep them open,
just as we’re
going to need to
subsidize COVID
testing and
other things.
But the cost of
not doing that
is even higher.
Not only is it
the cost for the
people getting
sick; we’re not
going to be able
to control the
epidemic and
reopen the
economy.
Q. One argument
made under Trump
is that there
were limited
resources for
inspection, so
how would OSHA
enforce this
stuff?
A. That’s
nonsense. OSHA
certainly could
have done the
job very
differently.
This agency,
which is filled
with dedicated
career
professionals,
was very
frustrated by
the Trump
administration.
I think you’ll
see a great deal
more out of OSHA
now, under
President Biden.
The 13 experts
who wrote the
letter —
including
several who
advised Mr.
Biden during the
transition —
urged the
administration
to blunt the
risks in a
variety of
workplaces by
requiring a
combination of
mask-wearing and
environmental
measures,
including better
ventilation.
They want the
C.D.C. to
recommend the
use of
high-quality
masks like N95
respirators to
protect workers
who are at high
risk of
infection, many
of whom are
people of color,
the segment of
the population
that has been
hit hardest by
the epidemic in
the United
States.
At present,
health care
workers mostly
rely on surgical
masks, which are
not as effective
against aerosol
transmission of
the virus as N95
masks are.
Mr. Biden has
directed the
Occupational
Safety and
Health
Administration,
which sets
workplace
requirements,
to issue
emergency
temporary
standards for
Covid-19,
including
those regarding
ventilation and
masks, by March
15.
Americans will
Still be Wearing
Masks in 2022
Dr. Anthony S.
Fauci, President
Biden’s chief
medical adviser
for Covid-19,
said on Sunday
that Americans
may still be
wearing masks
outside their
homes a year
from now, even
as he predicted
the country
would return to
“a significant
degree of
normality” by
fall.
“I want it to
keep going down
to a baseline
that’s so low
there is
virtually no
threat,” Dr.
Fauci said on
the CNN program
“State of the
Union,”
referring to the
number of cases
nationally that
would make him
comfortable
enough to stop
recommending
universal
masking. “If you
combine getting
most of the
people in the
country
vaccinated with
getting the
level of virus
in the community
very, very low,
then I believe
you’re going to
be able to say,
for the most
part, we don’t
necessarily have
to wear masks.”
Need to Focus on
Length of Mask
Use
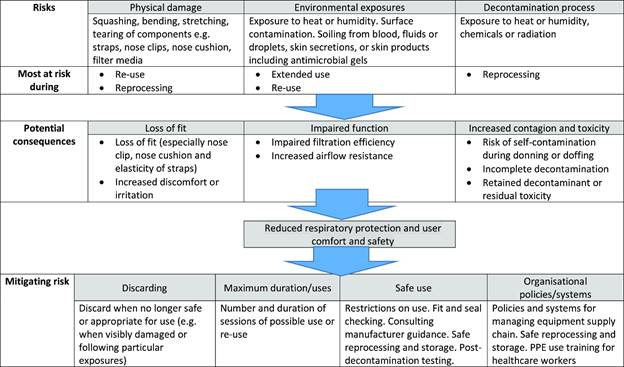
Most of the
academic studies
focus on
extended use and
reuse of masks
in medical
settings.
Medical
workers are
likely to be
exposed to COVID
at rates which
are much higher
than individuals
in public
settings. The
new ASTM
standards
address the
deterioration
rate for
reusable masks.
However, someone
who goes to the
store wearing a
mask and then
spends the rest
of the day in
his house
without a mask
may be wearing
the mask for
only an hour or
two per day.
The office
worker who wears
a mask all day
long will log
user hours at 5
to 20 times the
homebody who
goes out rarely.
The care with
which masks are
stored when not
in use is
another
variable.
Considerable
analysis is
needed in this
area. Some data
such as the
following table
will be useful
even though it
was designed for
medical workers.
The full
document is
found at
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7588721/
GW University
Creating HVAC
Systems Which
Minimize
Horizontal Air
Flow
George
Washington
University is
completing a
second phase of
HVAC upgrades in
several campus
buildings this
semester to
align with
COVID-19 safety
protocols and
limit energy
consumption.
David Dent, the
associate vice
president for
facilities
planning,
construction and
management, said
officials are
renovating the
HVAC systems in
Enterprise,
Phillips, Rome,
Discovery and
Ames halls,
Amsterdam House,
the Smith Hall
of Art and
Building GG
before June. He
said officials
upgraded eight
other
residential
buildings last
fall as part of
the ReStart initiative,
a project aimed
to bolster HVAC
systems on
campus.
The ReStart
Initiative,
which is running
this academic
year, helped
officials
determine that
all buildings on
campus are “safe
for occupancy.”
The project’s
first phase of
upgrades in the
fall cost GW
$2.4 million,
The project also
indicated that
officials need
to invest more
into mechanical
systems “to
address deferred
maintenance,”
Dent said. He
said officials
identified the
buildings that
needed more
modernization to
comply with the
University’s
standards for
carbon
footprint,
greenhouse gases
and energy
performance.
“You don’t want
to have a system
which creates
large horizontal
flows of air
because if you
have a
horizontal flow
of air with the
velocity, say
one meter per
second, what
will happen
again is if
someone is ill
and is giving
off the virus,
that virus will
be carried in
the airstream to
other people in
the room,”
Glicksman said.
Glicksman said
the University’s
installation of
the MERV 13
filter, which
blocks
contaminants,
“works quite
well” and meets
the standard of
ventilation
expected of most
buildings. He
said the filters
can stop all
particles beside
“the very
tiniest”
aerosols that a
high-efficiency
filter could
block.
“People are
doing what they
think is best,”
he said. “There
has not been
enough absolute
standard to say
this will
guarantee that
the building
will be
completely safe.
It’ll certainly
be safer and
reduce the
probability of
transmission
from one person
to another, but
that’s the state
of the art right
now.”
Forrest Meggers,
an assistant
professor of
architecture at
Princeton
University, said
the challenge
for implementing
HVAC upgrades
under COVID-19
guidelines is
the significant
energy demand to
ensure a maximum
amount of fresh
air is being
delivered inside
the buildings.
He said the
upgrades under
the guidelines
are often
followed by a
200 to 300
percent increase
in energy
demand.
“We probably
aren’t going to
stay at that
level, but it’s
really exposed
the sensitivity
of our carbon
emissions and
primary energy
demand to
heating and
cooling
buildings and
how the mode of
heating and
cooling that we
do, which in the
U.S. explicitly
tied to air
conditioning,”
Meggers said.
Meggers said
officials should
introduce a
radiant hydronic
system, a
heating method
that utilizes
running water
through pipes to
create heat, to
address the
heating and
cooling
components of
HVAC upgrades,
which he said
would ultimately
be more
efficient.
“You’d have to
think about it
as a campus for
HVAC systems
– ‘I can make
these great
upgrades and
make the
buildings more
comfortable and
a little bit
more efficient
by putting
water-based
heating and
cooling systems
and making the
ventilation be
more focused on
delivering care
efficiently and
having heat
recovery,'” he
said.
